Use has increased because of fear or not wanting to take a medication. Just know that quite a few who choose tissue valves for the lack of anti-coagulation end up on the anti-coag meds. You could get atrial fibrillation and end up getting prescribed Warfarin anyway.
a good point ...
I've edited this down from an editorial remark about the Edinburgh study (attached)
Edinburgh Study editorial
REOPERATION
What is clear is the increased requirement for reoperation in patients
implanted with bioprostheses.
Overall, 21% of the patients required reoperation during the follow up period,
but around four times more reoperations were performed in the bioprosthetic group
compared to the mechanical group.
The present study rightly draws attention to the not inconsiderable risks of
reoperation (15% at 30 days and 22% at one year following operation).
These data are consistent with the mortality rates following reoperation reported
in the UKHVR. Although much lower mortality rates for reoperative valve surgery
have been reported,5 6 overall experience with reoperative valve replacement
still indicates that this is a relatively high risk procedure, and should not be
undertaken lightly.
HAEMORRHAGE
The data from the current study would immediately confirm this perception;
particularly at 10 years postimplant
all bleeding episodes:
* 15% mechanical
* 7.5% bioprosthetic for
all major bleeding episodes
* 12% mechanical
* 5% bioprosthetic ).
The situation changes by 20 years, however, with a relative increase in the bioprosthetic group incidence of all major bleeding episodes.
One important factor to be taken into account, however, is the progressive increase in anticoagulant treatment in the bioprosthetic valve patient group with the passage of time:
at five years postoperatively,
15% of aortic
36% of mitral
bioprosthetic implantees were being treated with warfarin. By 15 years, the numbers had doubled.
If the decision is replacement rather than repair, the latest
results from the UKHVR,4 prospective since 1986, for
patients having mechanical valve replacements (n = 46 810)
compared to bioprosthetic implants (n = 25 977) report
survival at 15 years postoperation for
* mechanical valve patients of 47.4% (95% CI 46.3% to 48.6%)
* bioprosthetic valve patients of 30.3% (95% CI 29.0% to 31.6%).
This difference is at least partially explained by patient age at
the time of implant.
For those patients aged 70 years and over, the survival rates at 15 years
postimplant are virtually identical
* mechanical 20.2%, 95% CI 16.5% to 24.1%,
* bioprosthetic 16.6%, 95% CI 14.3% to 19.0%).
The study itself is
here (should verify that my PDF is not fabricated link) and as you can see it shows data from very old valves
The Edinburgh heart valve study of 533 patients, who had their valve implant(s) between 1975 and 1979, now reports comparative clinical outcome for mechanical versus bioprosthetic valves at 20 years.1 The present report supplements a 12 year follow up, published in 1991.2 The original study was prospective and randomised. The study design was modified in January 1977 in those patients randomised to receive a porcine bioprosthesis. Initially, the porcine valve used was the Hancock prosthesis, but, after January 1977, the Carpentier-Edwards valve was used because of its “substantial cost advantage”.
While on the subject:
d
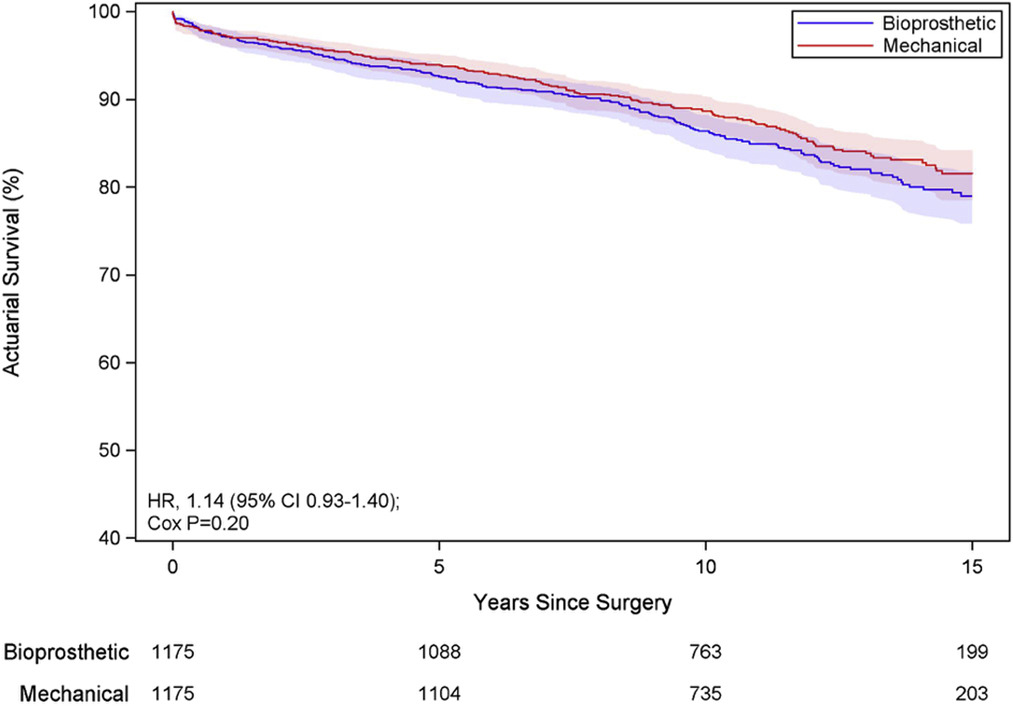
teapotimus quoted a study
valve but I recalled reading an interesting propensity matched study a while back that you may find helpful.
https://www.jtcvs.org/article/S0022-5223(17)31896-2/fulltext
which contained the following results
After bioprosthetic valve replacement (at 15 years versus mechanical valve replacement)
- stroke rates were lower 5.4% [95% CI, 3.8%-7.2%] vs 8.1% [95% CI, 6.3%-10.2%], HR 0.62 [95% CI 0.43-0.91]
- bleeding rates were lower 4.2% [95% CI, 3.0-5.6%] vs 8.4% [95% CI, 6.6-10.4%], HR 0.48 [95% CI, 0.33-0.69],
but reoperation rates were greater
- 24.5% [95% CI, 21.3%-27.8%] vs 9.3% [95% CI, 7.2%-11.7%],
HR 5.9 [95% CI 3.2-11.0])
For those unfamiliar with how to properly interpret Hazard Ratios from:
https://www.jto.org/article/S1556-0864(15)32030-X/fulltext
suggesting that both of the statistics on the stroke and the bleed rates (0.62 & 0.48 respectively) are below the threshold where one would really say they make much difference.
However the HR 5.9 for reoperation is well above 1.25
So basically he's just provided the data that makes the point in favor of mechanical
if you expect to live more than 15 years.
What
isn't mentioned is at 15 years how many of the bioprosthesis patients went on to needing ACT; which may elevated their rates of bleeds ... or didn't go on to ACT and that may have elevated their rates of strokes (where they didn't have reoperation before the 15 years but needed to go on to the very hing they sought to avoid... warfarin)
Also I'll take the red curve from that study thanks ...
Again, from that article
Discussion
... Our study indicates that aortic prosthesis choice appears to have minimal impact on survival at 15 years and suggests that bioprosthetic aortic valve replacement, which was associated with a lower risk of stroke and major bleeding, is a reasonable alternative to aortic mechanical valve replacement for adult patients younger than 50 years of age.
The primary benefit of mechanical over bioprosthetic aortic valve replacement in our analysis was the almost 60% reduction in reoperation at 15 years
Oh, is that all only a 60% reduction
Not a bad analysis for a guy without a high school education who taught himself to read (well, a couple of other languages if not English).