Wow! That's fantastic!! I was born that year so it's a good year!I've only had one OHS......in 1967 when my mechanical valve was implanted......and it's still clickin'.
You are using an out of date browser. It may not display this or other websites correctly.
You should upgrade or use an alternative browser.
You should upgrade or use an alternative browser.
Mechanical vs Tissue - need help deciding
- Thread starter Holley650
- Start date

Help Support Valve Replacement Forums:
This site may earn a commission from merchant affiliate
links, including eBay, Amazon, and others.
............ How has it been taking blood thinners?
You put the pill in your mouth and wash it down with water
1. Take the anti-coagulant (warfarin) as prescribed!!! A seven-day pill box makes this easy.
2. Test your (INR) regularly....every week or two....10 minute home testing is now common practice.
3. Don't run with scissors. Anyone who can walk and chew gum at the same time can co-exist with warfarin.
You put the pill in your mouth and wash it down with water. Seriously, my problems with warfarin have been limited to only one time.......I allowed my blood to get too close to normal and I suffered a stroke. That was almost 50 years ago and I have had no problem with warfarin (blood thinner) since. I have three "ironclad rules" that I follow:
1. Take the anti-coagulant (warfarin) as prescribed!!! A seven-day pill box makes this easy.
2. Test your (INR) regularly....every week or two....10 minute home testing is now common practice.
3. Don't run with scissors. Anyone who can walk and chew gum at the same time can co-exist with warfarin.
It's definitely nice to know you won't need to go through OHS again! That's definitely a huge benefit to a Mechanical Valve. Glad you haven't had any issues after that one blip. I have talked to a few people who have said the same. It really hasn't been an issue for them. I don't run with scissors, thank God!
- Joined
- Dec 5, 2020
- Messages
- 2,895
I can tell you that the single biggest thing you can do to speed your recovery is to slow your recovery.
Agreed. Especially for folks who tend to be over achievers. It can be very tempting to start pushing too hard too soon, if one feels good. No need to rush. We have the rest of our lives to get back in top shape.
pellicle
Professional Dingbat, Guru and Merkintologist
Hi
agreed
gosh, well phrased!I can tell you that the single biggest thing you can do to speed your recovery is to slow your recovery.
agreed
pellicle
Professional Dingbat, Guru and Merkintologist
I know you asked Dick but "blood thinners" (and they aren't in any way thinning your blood) is really more in the mind than it is in reality. I can't count how many times people here have said:How has it been taking blood thinners?
I was really worried about it but it turned out to be a nothing.
I have a very detailed blog post on it here (as well as many other posts on things around life on warfarin).
The basic thing in making a valve choice is this: There is no cure for valvular heart disease, so what we do is to exchange valvular heart disease for "prosthetic valve disease". One is managed by keeping your blood coagulation levels managed (mechanical valve) the other is managed by repeat surgeries (tissue valve and may also result in you needing to manage your blood coagulation levels soo).
I would say that if you aren't going to take your simple task of taking your drug and monitoring your INR weekly then you will come to harm and your best served by a tissue prosthetic. I have had a repair of the aortic valve, a replacement homograft in the aortic position and lastly nearly 10 years ago a mechanical and a fix of an aneurysm.
One of the other benefits of a mechanical (aside from it being the only type that gives you a serious chance of never needing another surgery) is that once things are settled you may find that your need for monitoring decreases. This is the opposite situation of a tissue prosthesis which will require an increase in monitoring as it passes the 10 year mark and approaches what is called Structural Valve Degradation ... SVD is pretty much a certainty for a tissue valve.
Just search here for the amount of people who got less than their "rosy glasses view" ... oh, and the more active you are the more a tissue prosthesis is likely to enter SVD earlier than later.
Eg
Greetings, I had a St Jude Trifecta implant in 2015 and now find myself in need of a replacement due to deterioration.
very sad ...
I hear time and time again "but I'm active, I can't have a mechanical valve"
https://www.newsweek.com/my-turn-climbing-everest-bionic-heart-99749
hard to better that for activity

$28.91 ($0.32 / Count)
NutraPro Healthy Heart - Heart Health Supplements. Artery Cleanse & Protect. Supports Healthy Cholesterol and Triglyceride. GMP Certified
Gulliver Group

$91.95 ($0.34 / Count)
Snap Supplements Heart Health Supplements and Blood Circulation Supplements, 270 Capsules
SnapSupplements
Interesting - my reading/surgeon indicated that I'll buy more time from my tissue valve by being active than by riding the couch.oh, and the more active you are the more a tissue prosthesis is likely to enter SVD earlier than later.
I know you're a data guy, so if you have any links handy, I'd appreciate it. If not, no problem, I'll just dig deeper.
Another minor data point - had a consult w/ the shoulder surgeon and he basically flat out said that at my age, a full shoulder replacement was a no-go if I were on blood thinners. They'd arthro as best they could, but wouldn't take the chance on the open shoulder surgery.
I completely agree that the mechanical is a better choice for lots of people, but if you expect a knee/hip/any other major surgeries, it's important to think hard about the tissue valve.
pellicle
Professional Dingbat, Guru and Merkintologist
he's right ... but not only from the tissue (from health), and define "active"Interesting - my reading/surgeon indicated that I'll buy more time from my tissue valve by being active than by riding the couch.
Doctors (surgeons included) seem to not really deeply engage with you and your lifestyle.
With respect to data I'm driven by what I see mentioned (almost as an aside) in every paper I read (no, I don't just read the "conclusions" and "abstract") But here's one for you which is neutral
https://www.acc.org/latest-in-cardi...sthetic-valve-durability-incidence-mechanisms
I encourage you to search the boards here (with a good google search such as this, or similar key words)
This link is a good starter, consult points 7 and 8 (which does not directly address that specific aspect of the question.
Another minor data point - had a consult w/ the shoulder surgeon and he basically flat out said that at my age, a full shoulder replacement was a no-go if I were on blood thinners. They'd arthro as best they could, but wouldn't take the chance on the open shoulder surgery.
now that is something which is really out of my depth ... I've had minor surgeries (well and some debridements) on ACT, but that may be different.
I bridle when I hear "blood thinners" because it implies an ignorance of what's happening (and thinning isn't one of them).
Some links I found in a quick dig. The implication for all of the readings is that SVD is just going to happen (NB The biological tissue from both surgical and transcatheter bioprostheses is prone to structural valve degeneration (SVD) ) (cited from this link but the whole thing is worth a view)
I interpret this as meaning inflammation reactions such as are common as a side effect of high activity " ...In addition to this passive degenerative process, several studies have suggested active mechanisms that trigger inflammatory responses that are followed by calcification "
My understanding is supported by studies like this:
https://www.frontiersin.org/articles/10.3389/fphys.2019.01550/full
Exercise leads to a robust inflammatory response mainly characterized by the mobilization of leukocytes and an increase in circulating inflammatory mediators produced by immune cells and directly from the active muscle tissue. Both positive and negative effects on immune function and susceptibility to minor illness have been observed following different training protocols. While engaging in moderate activity may enhance immune function above sedentary levels, excessive amounts of prolonged, high-intensity exercise may impair immune function.
Perhaps someone with a better knowledge of exercise physiology would care to comment (@leadville thoughts?) on the accuracy of my assumption here.
Lastly I'll say that almost no studies or data is around that focuses on (even amateur) athletes and their bio-prostheses and nobody in health is going to say "don't live a healthy lifestyle with good exercise"
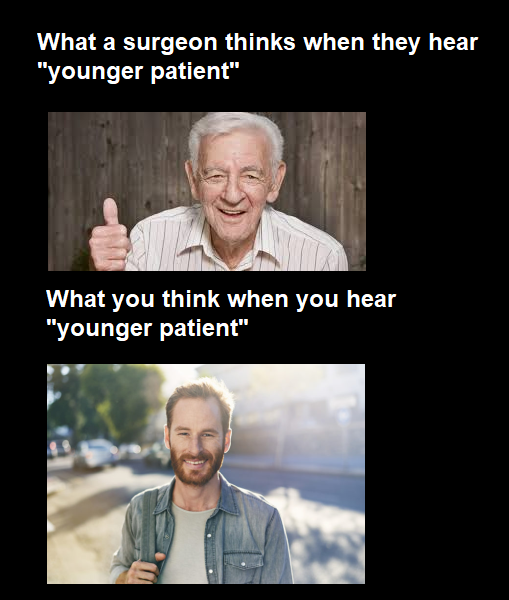
wever, SVD limiting valve durability continues to be one of the main limitations of biological (vs. mechanical) valves ... Valve leaflet calcification has been recognized as the primary mechanism responsible for SVD, and the factors associated with an increased risk are related to patient characteristics (younger age, larger body mass index), cardiovascular risk factors, and variables pertaining to bioprosthetic valves per se (increased transvalvular gradient, prosthesis-patient mismatch). Although the reported durability of surgical aortic bioprosthesis is >85% at 10 years, most studies to date have used reoperation instead of valve performance parameters to define valve durability
Lastly: this is something I have picked up over the years and I've simply not gathered a bibliography on it because I've really focused my research on me ... and I was entirely certain (as we my surgeon) that my homograft replacement would NOT be a tissue prosthesis having my 3rd surgery at the age of 48.
HTH
Last edited:
Fair point re: "blood thinners" - I was being sloppy. I have noticed and it does bug me that even the local coumadin clinic staff use the phrases blood thinners/clotting factors interchangeably.
" Doctors (surgeons included) seem to not really deeply engage with you and your lifestyle. " Submitted for understatement of the year.
re: high intensity exercise - just dawned on me that the cortisol reaction from high intensity/inadequate rest may also contribute to SVD.
I appreciate the time you've taken to respond in detail. This helps a lot. I have a lot of reading to do.
" Doctors (surgeons included) seem to not really deeply engage with you and your lifestyle. " Submitted for understatement of the year.
re: high intensity exercise - just dawned on me that the cortisol reaction from high intensity/inadequate rest may also contribute to SVD.
I appreciate the time you've taken to respond in detail. This helps a lot. I have a lot of reading to do.
pellicle
Professional Dingbat, Guru and Merkintologist
Good morning (just got back from collecting insects and getting attacked by birds AKA morning bicycle ride)

(*sadly shotgun not allowed)
I do my best not to be triggered by it

I'm not always successful ...
thank you

I'm glad that I can contribute to a new path of thought. I personally never want anyone to simply accept my view, I prefer robust discussion (that causes me to think about if what I think is correct or what they've said is ...)
You may find some interesting discussion here too ...
it is of course older and you may have already watched it, but it does provide pause to reflect.
Lastly I'll say that people can't usually think statistically (which explains Vegas right there) and peacock facts to their preference. So I'll just leave a few pots here:
Best Wishes (now, its off to the shower that I've stopped sweating ... dam I wish there was something for that bird)

(*sadly shotgun not allowed)
Fair point re: "blood thinners" - I was being sloppy. I have noticed and it does bug me that even the local coumadin clinic staff use the phrases blood thinners/clotting factors interchangeably.
I do my best not to be triggered by it

I'm not always successful ...
" Doctors (surgeons included) seem to not really deeply engage with you and your lifestyle. " Submitted for understatement of the year.
thank you

re: high intensity exercise - just dawned on me that the cortisol reaction from high intensity/inadequate rest may also contribute to SVD.
I appreciate the time you've taken to respond in detail. This helps a lot. I have a lot of reading to do.
I'm glad that I can contribute to a new path of thought. I personally never want anyone to simply accept my view, I prefer robust discussion (that causes me to think about if what I think is correct or what they've said is ...)
You may find some interesting discussion here too ...
it is of course older and you may have already watched it, but it does provide pause to reflect.
Lastly I'll say that people can't usually think statistically (which explains Vegas right there) and peacock facts to their preference. So I'll just leave a few pots here:
- most AVR's now are tissue and that ratio is increasing
- TAVR is becomming more common
- inadequate managing of blood thinners will lead you to permanent harm
- mechanical valves require some more adjustment in your life (I mean especially now that you're already been in the wating room and going to have scans and checkups is the new normal
- taking a pill each day reminds me I have a heart condition
Best Wishes (now, its off to the shower that I've stopped sweating ... dam I wish there was something for that bird)
- Joined
- Dec 5, 2020
- Messages
- 2,895
I bridle when I hear "blood thinners" because it implies an ignorance of what's happening (and thinning isn't one of them).
My release documents from UCLA even referred to Coumadin as a blood thinner. You would think that they would know better
- Joined
- Dec 5, 2020
- Messages
- 2,895
Here are some publications by Pibarot et all regarding factors which have been shown to correlate with acceleration of bioprosthetic valve SVD - Structural Valve Deterioration. Dr. Pibarot is a cardiologist and researcher in Canada who has had many publications regarding valve disease.
Attachments
pellicle
Professional Dingbat, Guru and Merkintologist
this is exactly what I'm on about !!!ou would think that they would know better
pellicle
Professional Dingbat, Guru and Merkintologist
the two seem to be the one ...Here are some publications by Pibarot et all regarding factors which have been shown to correlate with acceleration of bioprosthetic valve SVD - Structural Valve Deterioration. Dr.
krosson62
Active member
- Joined
- Nov 15, 2020
- Messages
- 26
A year ago August I had an artificial mitral valve replacement. I heard the ticking I think it was the 3rd day after surgery. It didnt scare me or worry me at all honestly it was a welcome tick without it I may not be hearing my son's laugh, my husband's occasional growl, or my grandaughters saying love u Grammy. I hear the tick now at least once every couple days. The only people I know besides myself that have heard it are docs or nurses.I'm a 48 year old male; 6'-3" height and 275lb.
I have AVR in my very near future, and need to decide my path forward : Mechanical (On-X) valve or Tissue valve.
I'm very nervous about the prospect of hearing something tick in my chest for the rest of my life.
Is there anyone out there that can shed some light on the noise concern - and perhaps share their experience?
Any feedback / recommendations greatly appreciated
Holley650
(because I feel like I'm having a carburetor serviced on a V-8 engine)
- Joined
- Dec 5, 2020
- Messages
- 2,895
Thanks. Will upload the other when I get back to my PCthe two seem to be the one ...
- Joined
- Dec 5, 2020
- Messages
- 2,895
Just uploaded the other document. Thanks for the head upthe two seem to be the one ...
What are the chances you end up on blood thinners in your 60s?
What are the chances you develop afib from the surgeon slicing your heart?
What are the chances you need another open heart surgery before you are TAVR ready?
What would your financial situation be at that point and time?
I love wellness visits with my doctor. We catch up and make plans for the coming year. I hate sick visits. I hate hospitals.
I only want to know what can we do so that I don't come in here again or reduce the chances of having to do this ever again.
What are the chances you develop afib from the surgeon slicing your heart?
What are the chances you need another open heart surgery before you are TAVR ready?
What would your financial situation be at that point and time?
I love wellness visits with my doctor. We catch up and make plans for the coming year. I hate sick visits. I hate hospitals.
I only want to know what can we do so that I don't come in here again or reduce the chances of having to do this ever again.
You are missing out on life. I stop kids putting things in their mouths with a story about how I swallowed my daddy's favorite watch and they can hear it for themselves.A year ago August I had an artificial mitral valve replacement. I heard the ticking I think it was the 3rd day after surgery. It didnt scare me or worry me at all honestly it was a welcome tick without it I may not be hearing my son's laugh, my husband's occasional growl, or my grandaughters saying love u Grammy. I hear the tick now at least once every couple days. The only people I know besides myself that have heard it are docs or nurses.
And the know it all adults who say is that your pacemaker ticking? NO! I have a mechanical heart. They do make them. I charge it up once a month.
pellicle
Professional Dingbat, Guru and Merkintologist
Gosh this is worth reiterating in decision making:
I have variously made all those points many times across many hundreds of discussions here.
As Jordan Peterson mentions, you have to make decisions about not just yourself, but about yourself in 10 years, yourself in 20 years ... not to mention decisions that take into account those in your immediate family. However not many grasp the reasons for financial planning either.

Lastly, I would point out though that another surgery before TAVR would mean that any valve may be explanted and replaced, but the real kicker is to find that you are not suitable for TAVR and have to get another valve. Also I'd add that some percentage of tissue valves begin thrombosis issues as they enter SVD and so you may find yourself on Warfarin less than 10 years into your "I avoided warfarin choice"
Best Wishes
What are the chances you end up on blood thinners in your 60s?
What are the chances you develop afib from the surgeon slicing your heart?
What are the chances you need another open heart surgery before you are TAVR ready?
What would your financial situation be at that point and time?
I have variously made all those points many times across many hundreds of discussions here.
As Jordan Peterson mentions, you have to make decisions about not just yourself, but about yourself in 10 years, yourself in 20 years ... not to mention decisions that take into account those in your immediate family. However not many grasp the reasons for financial planning either.

Lastly, I would point out though that another surgery before TAVR would mean that any valve may be explanted and replaced, but the real kicker is to find that you are not suitable for TAVR and have to get another valve. Also I'd add that some percentage of tissue valves begin thrombosis issues as they enter SVD and so you may find yourself on Warfarin less than 10 years into your "I avoided warfarin choice"
Best Wishes











