Warfarin is taken for essentially two reasons following mechanical valve surgery. First if no anticoagulants are used the valve may clot and lock up.
Second small emboli form around the valve or through areas of irregular flow through the valve. These emboli travel downstream and sometimes lodge in some blood vessel. Depending on which vessel determines the symptoms.
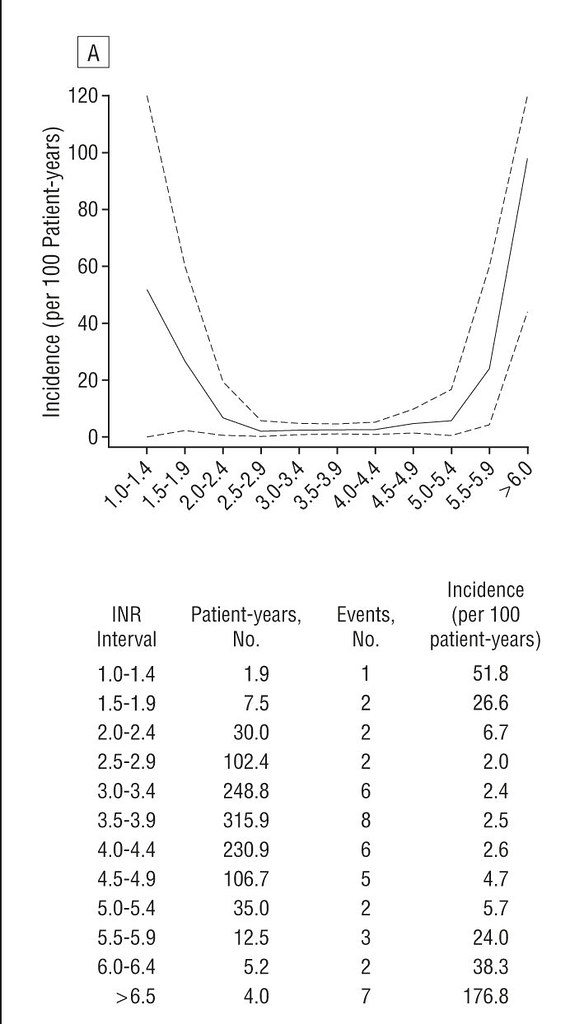
If the embolus is small it can brake up and the symptoms diminish hence a TIA. In my case I have had small transient blockages in retinal vessels where part of my visual field goes dark in one eye. Fortunately all have passed usually within 5 or so minutes. This is not migraine which affects the field in both eyes. But any part of the brain can be affected so many different symptoms could occur. Anticoagulants markedly decrease the chance of these events but like many things in medicine they don’t eradicate them.The recommendations for INR levels are based on a balance of reducing vascular issues vs increasing your possible hemorrhagic issues. Probably no microparticles from the valve but the mesh on the valve gets covered by tissue growth after several months and this could decrease potential emboli.
Second small emboli form around the valve or through areas of irregular flow through the valve. These emboli travel downstream and sometimes lodge in some blood vessel. Depending on which vessel determines the symptoms.
If the embolus is small it can brake up and the symptoms diminish hence a TIA. In my case I have had small transient blockages in retinal vessels where part of my visual field goes dark in one eye. Fortunately all have passed usually within 5 or so minutes. This is not migraine which affects the field in both eyes. But any part of the brain can be affected so many different symptoms could occur. Anticoagulants markedly decrease the chance of these events but like many things in medicine they don’t eradicate them.The recommendations for INR levels are based on a balance of reducing vascular issues vs increasing your possible hemorrhagic issues. Probably no microparticles from the valve but the mesh on the valve gets covered by tissue growth after several months and this could decrease potential emboli.