pellicle
Professional Dingbat, Guru and Merkintologist
A discussion I had yesterday (@tezza ) led me to discuss a common concern that new warfarin takers ask:
"How long can I go without warfarin"
This is of course a question without specific answers (such as how long is a furlong {ans: 201.168Meters}), and a lot depends on various things. Which valve you have is important in this question because older ball and cage valves have different "risk profiles" associated with them than do modern bileaflet valves. So its not just about your risk factors as a person (some are inherently more likely to have a stroke than others as they age) but also about the valve you have.
I do not intentend to write a piece that suggests you go off warfarin for a long period, the aim of this piece is to allay fears that "dipping so much as a pinky" into the pond of "I missed a dose" will result in something reaching up and pulling you into the swamp of harm.
To return to the question "how long can you go". Well I'd start with this extreme example:
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4818019/
Event free:
Table 1
A summary of cases with long event-free survival in patients with mechanical valve replacement.
I recommend you read the rest of the article. But this alone should suggest to you that even 2 consecutive missed doses will perhaps be of low risk.
Next lets look at modern prescription views. I have twice now dipped my pinkie into the pond of cessation of warfarin for the valid reason of perioperative safety. Especially when a risk of an extensive bleed is high (such as with a colonoscopy). Accordingly I wrote up my experiences here:
http://cjeastwd.blogspot.com/2017/12/perioperative-management-of-inr.html
and wrote that based on an analysis of this article: The perioperative management of anticoagulation
I wrote there that the risks are difficult to quantify due to the lack of randomised trials examining this issue. They vary according to the indication for the warfarin therapy, and cited:
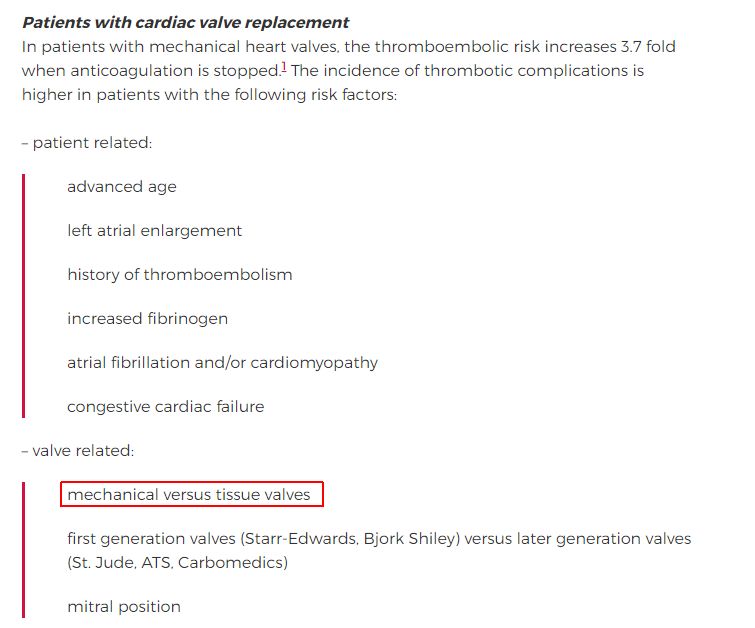
which shows that modern bileaflet aortic valvers are among the lowest risk factors
Its interesting that while on the one hand people will be clear that "adjustment of dose takes time to appear in the INR" (which is the measure of thrombogenesis") yet are concerned about their INR when they are in a different metal context (what if I miss a dose)
So I took the opportunity to actually measure for myself (not the first time I'd done this btw), and I got this
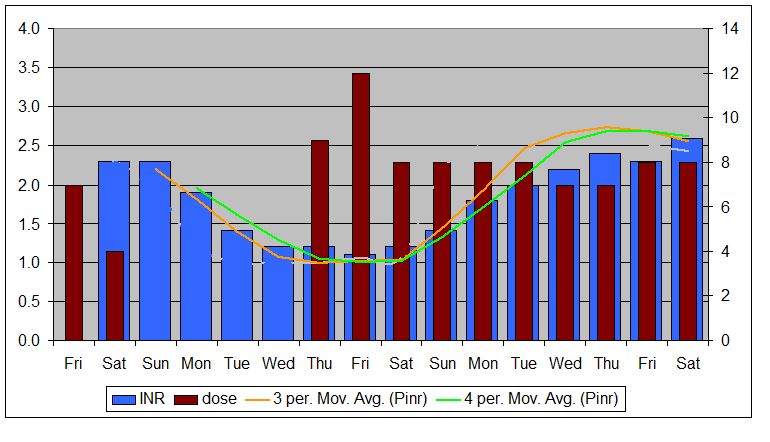
as you see it took some time to drop (and also some time to rise again). {Note: the Pinr in that graph is my "Predicted INR" based on my data model.
You can see that I took a half dose on Saturday (I don't really know why I chose that), then nothing for Sunday, Monday, Tuesday and Wednesday. That's a lot of missed doses and I having a colonoscopy took no aspirin for a week before that too.
No events.
The finding of the article I cited is that : " The need for perioperative anticoagulation in patients with mechanical heart valves has been questioned in a recent review. The authors argue that for every 10 000 patients with mechanical heart valves who are given perioperative intravenous heparin, three thromboembolic events are prevented at the cost of 300 major postoperative bleeding episodes "
so the picture is emerging that the prior emphasis on coagulation is perhaps an over reaction, perhaps resulting from inadequate evaluation of actual needs of patients. Indeed over time study after study is supporting that lower INR's are possible (so case #2's bruising can probably go off the list of problems) and technology is allowing us (valvers) to more accurately and more consistently measure our INR (especially important for anyone hovering on a lower INR)
What I think this means is that some of the veil of ignorance based fear can be lifted and we can breath a little easier.
I encourage you to read that post in detail and consider again if a fear of missing a dose is justified by the data.
Best Wishes
"How long can I go without warfarin"
This is of course a question without specific answers (such as how long is a furlong {ans: 201.168Meters}), and a lot depends on various things. Which valve you have is important in this question because older ball and cage valves have different "risk profiles" associated with them than do modern bileaflet valves. So its not just about your risk factors as a person (some are inherently more likely to have a stroke than others as they age) but also about the valve you have.
I do not intentend to write a piece that suggests you go off warfarin for a long period, the aim of this piece is to allay fears that "dipping so much as a pinky" into the pond of "I missed a dose" will result in something reaching up and pulling you into the swamp of harm.
To return to the question "how long can you go". Well I'd start with this extreme example:
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4818019/
Event free:
- case 1 = 13 years
- case 2 = 35 years
Table 1
A summary of cases with long event-free survival in patients with mechanical valve replacement.
CASES | AGE | POSITION | TYPE | YEARS |
|---|---|---|---|---|
Kucukaksu et al.19 | 56 | Aortic | B-S | 30 |
Uzun et al.23 | 45 | Aortic | S-E | 2 |
Yildiz et al.20 | 42 | Aortic | B-S | 22 |
Ozkokeli et al.21 | 58 | Aortic | S-E | 37 |
Ikizler et al.22 | 58 | Aortic | S-E | 34 |
Sharma et al.23 | 68 | Aortic | St Jude | 23 |
Björk et al.16 | – | Mitral | – | – |
Perez-Zaldivar et al.14 | 26 | Mitral | St Jude | 10 |
Cicekcioglu et al.24 | 21 | Tricuspid | B-S | 15 |
Iscan hz et al.25 | 25 | Pulmonary | St Jude | 15 |
Enes et al.5 | 46 | Mitral | St Jude | 27 |
Present case 1 | 92 | Aortic | – | 23 |
Present case 2 | 66 | Aortic | B-S | 35 |
I recommend you read the rest of the article. But this alone should suggest to you that even 2 consecutive missed doses will perhaps be of low risk.
Next lets look at modern prescription views. I have twice now dipped my pinkie into the pond of cessation of warfarin for the valid reason of perioperative safety. Especially when a risk of an extensive bleed is high (such as with a colonoscopy). Accordingly I wrote up my experiences here:
http://cjeastwd.blogspot.com/2017/12/perioperative-management-of-inr.html
and wrote that based on an analysis of this article: The perioperative management of anticoagulation
I wrote there that the risks are difficult to quantify due to the lack of randomised trials examining this issue. They vary according to the indication for the warfarin therapy, and cited:
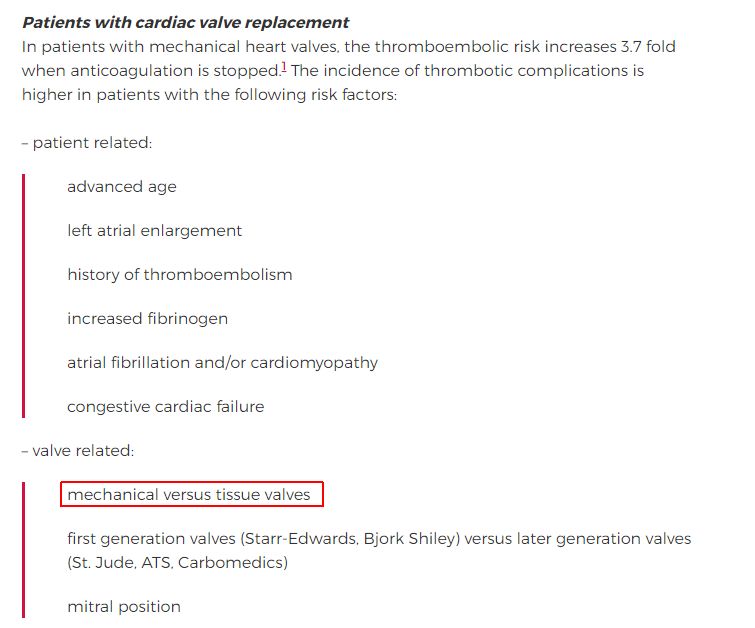
which shows that modern bileaflet aortic valvers are among the lowest risk factors
Its interesting that while on the one hand people will be clear that "adjustment of dose takes time to appear in the INR" (which is the measure of thrombogenesis") yet are concerned about their INR when they are in a different metal context (what if I miss a dose)
So I took the opportunity to actually measure for myself (not the first time I'd done this btw), and I got this
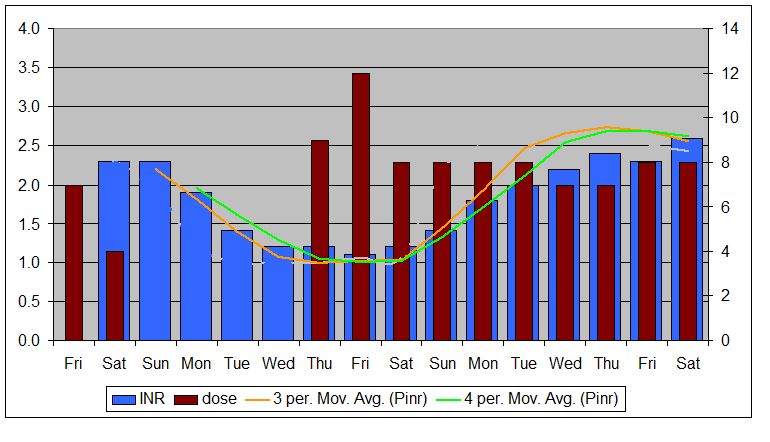
as you see it took some time to drop (and also some time to rise again). {Note: the Pinr in that graph is my "Predicted INR" based on my data model.
You can see that I took a half dose on Saturday (I don't really know why I chose that), then nothing for Sunday, Monday, Tuesday and Wednesday. That's a lot of missed doses and I having a colonoscopy took no aspirin for a week before that too.
No events.
The finding of the article I cited is that : " The need for perioperative anticoagulation in patients with mechanical heart valves has been questioned in a recent review. The authors argue that for every 10 000 patients with mechanical heart valves who are given perioperative intravenous heparin, three thromboembolic events are prevented at the cost of 300 major postoperative bleeding episodes "
so the picture is emerging that the prior emphasis on coagulation is perhaps an over reaction, perhaps resulting from inadequate evaluation of actual needs of patients. Indeed over time study after study is supporting that lower INR's are possible (so case #2's bruising can probably go off the list of problems) and technology is allowing us (valvers) to more accurately and more consistently measure our INR (especially important for anyone hovering on a lower INR)
What I think this means is that some of the veil of ignorance based fear can be lifted and we can breath a little easier.
I encourage you to read that post in detail and consider again if a fear of missing a dose is justified by the data.
Best Wishes
Last edited:














