Hi. Long time since I've been on. Hope everyone is doing well and that newcomers are getting the great support I got when I first signed on.
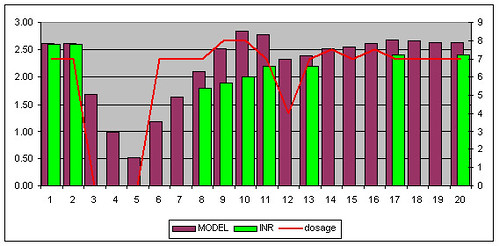
It turns out that when I home tested on the 15th (Friday - 3 days ago), my INR was 2.2. I had been taking 8.5mg/day. So I bumped it up to 9mg/day beginning Friday night. I took 9mg Friday, 9mg Saturday, and the FORGOT on Sunday. I just realized this tonight when I went to take my medicine. So I measured my INR. It is 1.7. This makes me a bit nervous, especially since I was already low out of range on Friday and have been trying to boost it up. So tonight (about an hour ago), I took my usual 9mg and then decided to take an extra 5mg (doubling up is contra-indicated, so I took 1.5 times the usual), and then I'll plan to make up the rest tomorrow and the next day. Does that make sense?
Also, given that my INR is so low (1.7) should I consult my doctor tonight about bridging with heparin (which I have at home)?
Appreciate any suggestions on this.
Thanks,
pem
It turns out that when I home tested on the 15th (Friday - 3 days ago), my INR was 2.2. I had been taking 8.5mg/day. So I bumped it up to 9mg/day beginning Friday night. I took 9mg Friday, 9mg Saturday, and the FORGOT on Sunday. I just realized this tonight when I went to take my medicine. So I measured my INR. It is 1.7. This makes me a bit nervous, especially since I was already low out of range on Friday and have been trying to boost it up. So tonight (about an hour ago), I took my usual 9mg and then decided to take an extra 5mg (doubling up is contra-indicated, so I took 1.5 times the usual), and then I'll plan to make up the rest tomorrow and the next day. Does that make sense?
Also, given that my INR is so low (1.7) should I consult my doctor tonight about bridging with heparin (which I have at home)?
Appreciate any suggestions on this.
Thanks,
pem