Hi everyone,
I am almost 4 weeks post op and as a followup to get my body acclimated to coumadin I am getting my INR checked every Tuesday. When I left the hospital after my surgery I was at 1.9 and since my first check in it has been a low 1.3 and has not changed.
Err ... well so what have you done about it? Has your dose changed?
The INR response to warfarin (coumadin is just a brand of that chemical) varies, both from person to person and within that person as over factors change. This is why regular measuring is required to keep the dose to what your body is doing.
Ask a diabetic if they take the same dose of insulin all the time and they will probably laugh and say, "that's not now it works"
At first I was being conservative to vitamin K and moderating portions, but now I have all but eliminated it just to see a change. I have checked all foods, vitamins, and medications for any conflicts and I have also began drinking a beer or two a day to assist with the thinning.
The beer a day is a good thing

, but will have zero effect in coagulation. Personally I hate the word thinning as the viscosity of your blood does not change, only the time taken to form clots.
That the vitamin K reduction didn't change it suggests you weren't taking enough to be effecting the system either.
The nurse and doctor at the coumadin clinic say that some people are more resilient to coumadin and I've read enough on this forum to see that it is not uncommon at all to take 3 weeks to get normal, but I understood that to be more of a high/low range INR and getting it to settle.
Basically there a few gene types that have different metabolisms of warfarin (meaning the ability to break it down and get rid of it), these are dependent on a gene labeled CYP2C9. This will effect how much you need. Testing for that gene is sort of pointless because dosage will ultimately be done by measuring the INR and deciding on a dose
Too low = administer more
Just right = leave dose same
Too high = reduce dose
Naturally there are delays and holdbacks on that so as you don't yo-yo your INR all over the place like a kid doing a burnout on a road.
My dosage has been raised twice and I am now alternating 7.5 and 10 mg doses daily.
Can anyone speak to a similar experience?
My dose varied from 4mg a day in hospital and crept up to 9 at one point and lately has been abut 7.5. Essentially I don't worry about what dose I need, just my INR.
Now I'm just putting on my asbestos suit here (in preparation for some heat) but calling it as I see it I have seen the worst mixed up confused approaches to warfarin doses ever when I read how some people do it. So without going into details about what I think is wrong I will suggest what I think of as right.
Only ever think in terms of daily dose, as you have so far suggested. Keeping that as even as possible will help you to observe and manage it. Personally I feel that alternated doses with significant bariations between the doses (like some people report 7 once a week and 5 others) will cause measurement related mistakes.
Make the alterations to your dose small. To allow this choose to have a variety of pill dose sizes on hand. They are colour coded to make it easy to see which is which. For instance I alternate between 7 and 7.5 at the moment. My pill sizes are
1, 3 and 5, so I take some half pills (they have a line to make breaking with your fingernail easy).
half a 1 + half a 3 + a 5 = 7
half a 5 + a 5 = 7.5
So my variation is 0.5mg between doses.
Now, there is a cumulative effect in warfarin because it does not disappear from your system as fast as you are adding it so that to see the effect of a dose you need to settle in. So wait at least a few days or perhaps a week before reading again and making any significant change.
Next the way to make fine tuning adjustments and that is to look at on which days you take which dose. I have a pill box dispenser which has each day labelled. I put my doses in on Sunday morning (even though I choose sat morning to check my INR).
By taking the 7.5 on Monday, Wednesday, Friday (and 7mg the other days) I will settle on a lower INR than if I took alternating 7.5 / 7mg
If you are interested I can email you the spreadsheet that I use for my recording and some other bits on understanding the doses. PM me with your email if you want this.

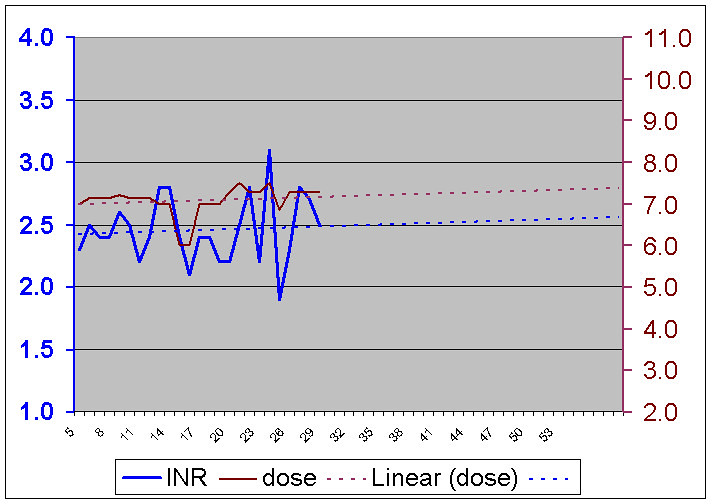
PS I thought I would put in a chart of my INR for some of this year. The measurements are done weekly and you can see the INR and the dose in mg.
You can also where I made a few bad judgement calls on reducing my dose and the change that occurred there. Sometimes the balance seems to get upset easily. This is by no means a highly unstable INR, its about what one would expect to find in the wild.
Which is of course why they give you a
range for your INR
Also, I have discovered when I get sick (a flu) that my required dose changes too.