Just had a bronchoscopy which required bridging with lovenox--my first time. My range is 2.5-3.5. I have a St Jude aortic valve. This is how it went. No Coumadin for 5 days before procedure--11/26 thru 11/30. Lovenox started on 3rd day 11/28. Procedure on 12/1. Restart Coumadin 12/1. Lovenox thru 12/3. 12/3 inr 1.2. 12/4 inr 1.4. Today 12/5 am inr still only 1.5. No lovenox since 12/3 pm. I'm concerned. Should I be? Weekend--doctors not available. What should I do?
You are using an out of date browser. It may not display this or other websites correctly.
You should upgrade or use an alternative browser.
You should upgrade or use an alternative browser.
Bridging with lovenox
- Thread starter mecretired
- Start date

Help Support Valve Replacement Forums:
This site may earn a commission from merchant affiliate
links, including eBay, Amazon, and others.
W. Carter
Well-known member
I'm no doctor and please don't do as I did without talking to your anticoagulation clinic. The last time I bridged they had me start my usual dose of warfarin the day after the surgery, and inject myself with 0.9 ml. of lovenox 6 straight days (once a day in the morning) after surgery. My inr checked at around 3.0 a week after surgery if my memory serves me right.
pellicle
Professional Dingbat, Guru and Merkintologist
Hi
hope the procedure went well. Without other information my first thought is that 2.5~3.5 range is higher than is recommended for a StJude aortic. That's more like Mitral valve guidelines. That factors into what I'll say next
so logically your INR was likely 1 (meaning uncoagulated) at that time. Like everything coagulation is calculated risks. The surgeon (based on research to establish guidelines) considers that a low risk.
may I say that I hate these sdrawkcab dates they are hard to read
well first I don't think you should be significantly concerned. As to what you should do, lets talk about your INR, what was your dose before the surgery, what is your dose now?
How are you determining your INR?
1.5 is a little out of the standard guideline range for your valve so to me (again I want more information about any other reasons for that high INR target, like afib or previous stroke history...) you should perhaps elevate your dose of warfarin a bit (say by 15%) and keep an eye on your INR perhaps every 3 / 4 days. Pull back to previous known doses when it approaches 2.5
This is my thoughts.
Best Wishes
mecretired;n860885 said:Just had a bronchoscopy which required bridging with lovenox--my first time. My range is 2.5-3.5. I have a St Jude aortic valve.
hope the procedure went well. Without other information my first thought is that 2.5~3.5 range is higher than is recommended for a StJude aortic. That's more like Mitral valve guidelines. That factors into what I'll say next
This is how it went. No Coumadin for 5 days before procedure--11/26 thru 11/30.
so logically your INR was likely 1 (meaning uncoagulated) at that time. Like everything coagulation is calculated risks. The surgeon (based on research to establish guidelines) considers that a low risk.
may I say that I hate these sdrawkcab dates they are hard to read
Lovenox started on 3rd day 11/28. Procedure on 12/1. Restart Coumadin 12/1. Lovenox thru 12/3. 12/3 inr 1.2. 12/4 inr 1.4. Today 12/5 am inr still only 1.5. No lovenox since 12/3 pm. I'm concerned. Should I be? Weekend--doctors not available. What should I do?
well first I don't think you should be significantly concerned. As to what you should do, lets talk about your INR, what was your dose before the surgery, what is your dose now?
How are you determining your INR?
1.5 is a little out of the standard guideline range for your valve so to me (again I want more information about any other reasons for that high INR target, like afib or previous stroke history...) you should perhaps elevate your dose of warfarin a bit (say by 15%) and keep an eye on your INR perhaps every 3 / 4 days. Pull back to previous known doses when it approaches 2.5
This is my thoughts.
Best Wishes
I have a st Jude's mechanical mitral valve. Also have atrial fibrillations. Had my surgery in 2001 at Cleveland Clinic with Dr Cosgrove. He also put in a Cosgrove ring in my pulmonary valve. I take 6 mg of Coumadin for 5 days and 4 mg for 2 days. I stay between 2.5-3.5 for my therapeutical range. I had gall bladder surgery and bridged with Lovenox last summer. All went well. Had nothing the day of surgery, but began Lovenox next day and Coumadin. I now need parathyroid surgery and the surgeon will also bridge with Lovenox but I may have to be without protection 24 to 36 hours. I worry a lot about that. Do we worry too much? For me it's very scary.
W. Carter
Well-known member
Everyone that bridges is without anticoagulation for a day and a half. I start with lovenox 100 mg. twice a day on the Jan 31 for a procedure on Feb. 3rd. The last shot before the procedure 8am the day before, resume the morning after the procedure along with regular Warfarin dose for 6 days. So you are without anticoagulation for roughly 36 hrs. This is the 2nd time bridging for me and both the same. If you are being cut on your blood has to be at normal clotting factor or you WILL have bleeding problems that would be hard to control.Sheenas7;n862158 said:I have a st Jude's mechanical mitral valve. Also have atrial fibrillations. Had my surgery in 2001 at Cleveland Clinic with Dr Cosgrove. He also put in a Cosgrove ring in my pulmonary valve. I take 6 mg of Coumadin for 5 days and 4 mg for 2 days. I stay between 2.5-3.5 for my therapeutical range. I had gall bladder surgery and bridged with Lovenox last summer. All went well. Had nothing the day of surgery, but began Lovenox next day and Coumadin. I now need parathyroid surgery and the surgeon will also bridge with Lovenox but I may have to be without protection 24 to 36 hours. I worry a lot about that. Do we worry too much? For me it's very scary.
pellicle
Professional Dingbat, Guru and Merkintologist
Hi
a small point (but important)
bridging is changing AC type, not being without AC ... Lovenox is AC therapy (it is a Heparin which is an anticoagulant). There are people who do not bridge (such as low risk Aortic valve only patients with no other propensity for clotting such as Atrial Fib) and those patients are without AC therapy.
Google Lovenox and you'll get stuff like this:
a small point (but important)
W. Carter;n862168 said:Everyone that bridges is without anticoagulation for a day and a half. I start with lovenox 100 mg. twice a day on the Jan 31 for a procedure on Feb. 3rd. The last shot before the procedure 8am the day before, resume the morning after the procedure along with regular Warfarin dose for 6 days.
bridging is changing AC type, not being without AC ... Lovenox is AC therapy (it is a Heparin which is an anticoagulant). There are people who do not bridge (such as low risk Aortic valve only patients with no other propensity for clotting such as Atrial Fib) and those patients are without AC therapy.
Google Lovenox and you'll get stuff like this:
Lovenox (enoxaparin) is an anticoagulant that helps prevent the formation of blood clots.
Thank you for your comments.
Dodger Fan
Well-known member
I'm on a heparin iv right now. I had AVR on the 11th. (St. Judes mechanical). Pacemaker on the 15th (St. Judes). I went home on Sunday the 16th with a 2.7 inr. On the 21st after a few painful but happy days with my family I suffered some memory loss which terrified my wife. I kept asking if I had had heart surgery. She showed me my incisions and asked if I remember. I said yes and immediately asked if I had heart surgery again. I don't remember much of that day and I haven't had memory issues since. She took me to the closest emergency room. They did a ct and found what iooked like a pituitary bleed. I was transferred by ambulance to Scripps Green. A pituitary bleed causes loss of field of vision, hormone changes, and headache (not amnesia). They kept me in icu for 8 days (I was just moved to a quieter floor today). They let my inr get below therapeutic range while on a heparin drip and did dally ct scans. The ct scans are stable indicating not an active bleed. They want to do an mri but can't due to my pacemaker being brand new. In about a month I will likely have an mri to be sure the pituitary thing is not an issue. Meanwhile my inr was at 1.7 this morning. I'm hoping to be at 2.0 in the morning and go home Saturday. It's been a long couple of weeks. I think the amnesia was caused by trauma and 2 doses of general anesthesia in a week.
W. Carter
Well-known member
If you notice Sheenas7 said that (he or she) would be without protection for 24-36 hrs. That is correct, even though you bridge with Lovenox the anticoagulation effect only last 12 hrs. per syringe injection. With bridging you have a window of 36 hrs. that starts before and ends after the procedure that you are not protected. Your last injection before the procedure will be at 8am the day before so at 8pm that night your clotting factor will be normal. The first shot after the operation or procedure will be the day after at 8am. Therefore you are without protection for exactly 36 hrs. Just one of the risks you take to have a procedure or surgery on Warfarin therapy.pellicle;n862169 said:Hi
bridging is changing AC type, not being without AC ... Lovenox is AC therapy (it is a Heparin which is an anticoagulant). There are people who do not bridge (such as low risk Aortic valve only patients with no other propensity for clotting such as Atrial Fib) and those patients are without AC therapy.
W. Carter
Well-known member
Hang in there buddy, I went through quite a few problems (bleeds) when I started anticoagulation therapy also. Over time your body will adjust and your INR will be stable. It just takes time.Dodger Fan;n862176 said:I'm on a heparin iv right now. I had AVR on the 11th. (St. Judes mechanical). Pacemaker on the 15th (St. Judes). I went home on Sunday the 16th with a 2.7 inr. On the 21st after a few painful but happy days with my family I suffered some memory loss which terrified my wife. I kept asking if I had had heart surgery. She showed me my incisions and asked if I remember. I said yes and immediately asked if I had heart surgery again. I don't remember much of that day and I haven't had memory issues since. She took me to the closest emergency room. They did a ct and found what iooked like a pituitary bleed. I was transferred by ambulance to Scripps Green. A pituitary bleed causes loss of field of vision, hormone changes, and headache (not amnesia). They kept me in icu for 8 days (I was just moved to a quieter floor today). They let my inr get below therapeutic range while on a heparin drip and did dally ct scans. The ct scans are stable indicating not an active bleed. They want to do an mri but can't due to my pacemaker being brand new. In about a month I will likely have an mri to be sure the pituitary thing is not an issue. Meanwhile my inr was at 1.7 this morning. I'm hoping to be at 2.0 in the morning and go home Saturday. It's been a long couple of weeks. I think the amnesia was caused by trauma and 2 doses of general anesthesia in a week.
pellicle
Professional Dingbat, Guru and Merkintologist
Hi
Firstly I commented on your point that implied Lovenox not being anticoagulation, nothing else.
which is also not a cause for concern. INR will not reduce to 1 like a shot from a gun. It will gradually reduce. This is important because coagulation is actually a critical body function. Surgery requires coagulation to be restablished. If you notice the periods witihout coagulation are quite minor and will actually still be showing effects of anticoagulation
So 26th she withheld warfarin, so by 27th INR would be falling but not uncoagulated, by 28th she had started Lovenox (again I assume not just one hit)
then
seems very well managed to me ... anyway my main concern was to assist Sheenas7 from not feeling anxious and your wording seemed to add to anxiety not reduce it
Your assertions are similar to suggesting that a missed dose is "unprotected" when we know that's not the case. The half life of warfarin is about 2 days. Meaning that after 2 days half of the warfarin is still in your system.
To me the prupose of this forum is to try ones best to make people feel comfortable with facts, not worried with conjecture.
This is a graph of my INR (and some other bits) when I had my last surgery
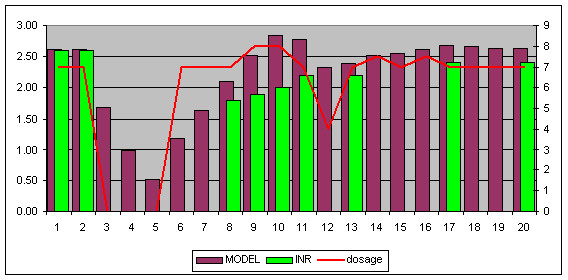
you can see that on days 3,4 and 5 I had no warfarin (red dose line). I was having INR tests done on the days with green bars. We both know that INR does not leap back up from 1 over a day to 1.5
Best Wishes
Firstly I commented on your point that implied Lovenox not being anticoagulation, nothing else.
W. Carter;n862180 said:If you notice Sheenas7 said that (he or she) would be without protection for 24-36 hrs.
which is also not a cause for concern. INR will not reduce to 1 like a shot from a gun. It will gradually reduce. This is important because coagulation is actually a critical body function. Surgery requires coagulation to be restablished. If you notice the periods witihout coagulation are quite minor and will actually still be showing effects of anticoagulation
No Coumadin for 5 days before procedure--11/26 thru 11/30.
Lovenox started on 3rd day 11/28.
So 26th she withheld warfarin, so by 27th INR would be falling but not uncoagulated, by 28th she had started Lovenox (again I assume not just one hit)
then
Procedure on 12/1. Restart Coumadin 12/1.
seems very well managed to me ... anyway my main concern was to assist Sheenas7 from not feeling anxious and your wording seemed to add to anxiety not reduce it
Your assertions are similar to suggesting that a missed dose is "unprotected" when we know that's not the case. The half life of warfarin is about 2 days. Meaning that after 2 days half of the warfarin is still in your system.
To me the prupose of this forum is to try ones best to make people feel comfortable with facts, not worried with conjecture.
This is a graph of my INR (and some other bits) when I had my last surgery
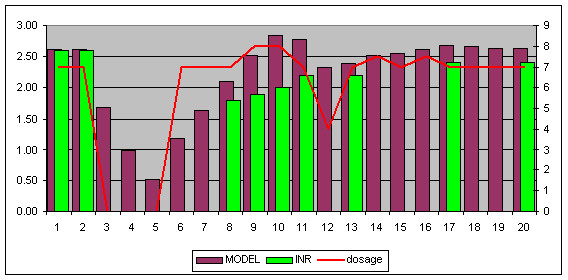
you can see that on days 3,4 and 5 I had no warfarin (red dose line). I was having INR tests done on the days with green bars. We both know that INR does not leap back up from 1 over a day to 1.5
Best Wishes
W. Carter
Well-known member
pellicle, You can argue with your hand if you want. You are unprotected for 36 HOURS. Now will that hurt most people, NO. When bridging you just don't stop Warfarin for 3 days like your graph, you stop it for 6 days where it is all out of your system three days before the operation. Lovenox shots just act for 12 hrs, then you need another shot to keep the anticoagulation working. I know that you are the expert at Warfarin therapy but maybe you need to study the effects of bridging a little closer. There is a reason that all anticoagulation medicine is evacuated the night before you get cut on and not started again until the next morning after surgery or procedure, LESS BLEEDING.
Best Wishes
Best Wishes
pellicle
Professional Dingbat, Guru and Merkintologist
of course ... naturally your totally right ... what else could you be?
Hi everyone. I appreciate the comments. I am not sure this time what the pre-surgical instructions will be. My cardiologist had discussed only being off the Lovenox for 12 hours. I think that will probably not happen. He said parathyroid surgery is almost bloodless. It depends what she (surgeon) has to do. If it is just one gland, or two or more. It is a benign adenoma (maybe more than one). It is not letting me absorb calcium which is causing a problem. I know I will be off Coumadin for probably 5 days, bridging of course with Lovenox which covers you for 12 hours and quickly dissipates, unlike Coumadin. But my concern are for the one or two days after surgery when you are totally unprotected. I believe my cardiologist said I need to narrow that margin as much as possible. He figured one stroke per 1000, if you are off for 12 hours. So risks increase for 24, 36 and so on. Those are the facts they explained so that is why it is a cause of worry. Balance the risk of no surgery and bone osteoporosis versus surgery and 95% cure.
pellicle
Professional Dingbat, Guru and Merkintologist
Hi
firstly so that I get this straight in my head soon after surgery you'll resume warfarin again right?
None the less if you read the surgical guidelines around handling warfarin (while each establishment has its own slight variation) the common theme is to divide patients into two groups:
* high clotting risk
* low clotting risk
People with modern bi leaflet valves in the aortic position are considered low risk. (**** has a much older ball and cage type which are higher risk valve types). The risk evaluation has been iteratively changed over the decades to reevaluate required anti-coagulation levels based on experience (**** had his surgery nearly 4 decades ago and is still ticking thankfully).
If you read this link you'll see that if you are a low risk patient that being off anticoagulation for some days is considered not a high risk.
http://www.australianprescriber.com/magazine/23/1/13/6
Risk is like crossing the road without looking. If you live in a tiny town with low traffic the risk is low that you'll get hit by a car. If you live in New York it will be much higher.
It can be important for wound healing that you balance the risks. If you don't establish a nice clean wound heal quickly after surgery the site can be colonised by bacteria. That is also a problem (thus a risk).
I've had two post op surgeries since I was on warfarin. On both I was off warfarin from the morning of the surgery and did not get any heparin until I returned to the ward from ICU. So I was "unprotected" for a few days.
From everything I read (and I'm a science trained person) the risks of any clot formation are very low in such a short time. Also there are people who just don't take their warfarin at all and suffer no problems for years with these modern valves, thus the PROACT trials.
I think you'll be fine and that while I understand your anxiety I think (in this case) you should just have more faith in your medical team as to me it seems like they know what they are doing.
Best Wishes
Sheenas7;n862204 said:My cardiologist had discussed only being off the Lovenox for 12 hours...
He said parathyroid surgery is almost bloodless. It depends what she (surgeon) has to do. If it is just one gland, or two or more
...But my concern are for the one or two days after surgery when you are totally unprotected.
firstly so that I get this straight in my head soon after surgery you'll resume warfarin again right?
None the less if you read the surgical guidelines around handling warfarin (while each establishment has its own slight variation) the common theme is to divide patients into two groups:
* high clotting risk
* low clotting risk
People with modern bi leaflet valves in the aortic position are considered low risk. (**** has a much older ball and cage type which are higher risk valve types). The risk evaluation has been iteratively changed over the decades to reevaluate required anti-coagulation levels based on experience (**** had his surgery nearly 4 decades ago and is still ticking thankfully).
If you read this link you'll see that if you are a low risk patient that being off anticoagulation for some days is considered not a high risk.
http://www.australianprescriber.com/magazine/23/1/13/6
Risk is like crossing the road without looking. If you live in a tiny town with low traffic the risk is low that you'll get hit by a car. If you live in New York it will be much higher.
It can be important for wound healing that you balance the risks. If you don't establish a nice clean wound heal quickly after surgery the site can be colonised by bacteria. That is also a problem (thus a risk).
I've had two post op surgeries since I was on warfarin. On both I was off warfarin from the morning of the surgery and did not get any heparin until I returned to the ward from ICU. So I was "unprotected" for a few days.
From everything I read (and I'm a science trained person) the risks of any clot formation are very low in such a short time. Also there are people who just don't take their warfarin at all and suffer no problems for years with these modern valves, thus the PROACT trials.
I think you'll be fine and that while I understand your anxiety I think (in this case) you should just have more faith in your medical team as to me it seems like they know what they are doing.
Best Wishes
Thank you Pellicle. I think St Jude mitral valve is higher risk than other valves. I go off Coumadin for 5 days and begin to rebuild with Coumadin the night after and for a couple days I am given both Lovenox and Coumadin to bring me up. But I will be off everything for one or two days depending on what they decide. I have to just trust it will be okay. Thanks for commenting!
ClickerTicker
Clickin and Tickin
I had open repairs to both an inguinal and an umbillical hernia in October. With a Carbomedics MItral Valve I'm certainly considered high-risk - normally running my INR at the UK guidelines of 3.0 to 4.0.
When I previously had a hernia repaired, my cardiologist insisted on intravenous heparin cover - needless to say that meant quite a spell in hospital, about six days I think. This time the guidelines seemed to have changed somewhat and he hovered between IV heparin again or self-injecting with Enoxaparin - which I ended up doing. To summarize, the thinking seemed to be that as the hospital performing my hernia ops (not my cardiologist's) normally used Enoxaparin bridging - the risk from them miscalculating the IV heparin dose outweighed the slight safety advantage of using it.
Anyway, the regime (I normally test early in the morning) went along the lines of:
Op minus 6 .... last warfarin
Op minus 5 ..... no warfarin
Op minus 4 ..... no warfarin
Op minus 3 ..... no warfarin, 8am 120mg Enoxaparin
Op minus 2 ..... no warfarin, 8am 120mg Enoxaparin
Op minus 1 ..... no warfarin, 8am 120mg Enoxaparin
Day of op .......... no warfarin, 60mg Enoxaparin at 6pm (op was in morning)
Op plus 1 ......... 8am restart warfarin, 60mg Enoxaparin at 6pm
Op plus 2 -> 4 . 8am warfarin and 120mg Enoxaparin
One thing I discovered was that my CoaguChek XS test strips contain an anti-heparin agent meaning that its INR measurements are still accurate even if Enoxaparin is in the bloodstream. It meant I was able to self-test and self-dose whilst my warfarin took effect - a great reassurance and no trips to the vampire.
Of course your mileage may vary depending on valve, cardiologist and hospital - I'm just summarising my experience as best as I can.
When I previously had a hernia repaired, my cardiologist insisted on intravenous heparin cover - needless to say that meant quite a spell in hospital, about six days I think. This time the guidelines seemed to have changed somewhat and he hovered between IV heparin again or self-injecting with Enoxaparin - which I ended up doing. To summarize, the thinking seemed to be that as the hospital performing my hernia ops (not my cardiologist's) normally used Enoxaparin bridging - the risk from them miscalculating the IV heparin dose outweighed the slight safety advantage of using it.
Anyway, the regime (I normally test early in the morning) went along the lines of:
Op minus 6 .... last warfarin
Op minus 5 ..... no warfarin
Op minus 4 ..... no warfarin
Op minus 3 ..... no warfarin, 8am 120mg Enoxaparin
Op minus 2 ..... no warfarin, 8am 120mg Enoxaparin
Op minus 1 ..... no warfarin, 8am 120mg Enoxaparin
Day of op .......... no warfarin, 60mg Enoxaparin at 6pm (op was in morning)
Op plus 1 ......... 8am restart warfarin, 60mg Enoxaparin at 6pm
Op plus 2 -> 4 . 8am warfarin and 120mg Enoxaparin
One thing I discovered was that my CoaguChek XS test strips contain an anti-heparin agent meaning that its INR measurements are still accurate even if Enoxaparin is in the bloodstream. It meant I was able to self-test and self-dose whilst my warfarin took effect - a great reassurance and no trips to the vampire.
Of course your mileage may vary depending on valve, cardiologist and hospital - I'm just summarising my experience as best as I can.
W. Carter
Well-known member
They go by your weight for the Lovenox dose that you have to take. The first time I bridged they had me doing 1 syringe daily in the morning of 140 mg, i'm 6' and I weighed 180 lbs. Now the current dose i'm bridging at is 100 mg syringe twice a day because I put on 30 lbs.ClickerTicker;n862210 said:I had open repairs to both an inguinal and an umbillical hernia in October. With a Carbomedics MItral Valve I'm certainly considered high-risk - normally running my INR at the UK guidelines of 3.0 to 4.0.
When I previously had a hernia repaired, my cardiologist insisted on intravenous heparin cover - needless to say that meant quite a spell in hospital, about six days I think. This time the guidelines seemed to have changed somewhat and he hovered between IV heparin again or self-injecting with Enoxaparin - which I ended up doing. To summarize, the thinking seemed to be that as the hospital performing my hernia ops (not my cardiologist's) normally used Enoxaparin bridging - the risk from them miscalculating the IV heparin dose outweighed the slight safety advantage of using it.
Anyway, the regime (I normally test early in the morning) went along the lines of:
Op minus 6 .... last warfarin
Op minus 5 ..... no warfarin
Op minus 4 ..... no warfarin
Op minus 3 ..... no warfarin, 8am 120mg Enoxaparin
Op minus 2 ..... no warfarin, 8am 120mg Enoxaparin
Op minus 1 ..... no warfarin, 8am 120mg Enoxaparin
Day of op .......... no warfarin, 60mg Enoxaparin at 6pm (op was in morning)
Op plus 1 ......... 8am restart warfarin, 60mg Enoxaparin at 6pm
Op plus 2 -> 4 . 8am warfarin and 120mg Enoxaparin
One thing I discovered was that my CoaguChek XS test strips contain an anti-heparin agent meaning that its INR measurements are still accurate even if Enoxaparin is in the bloodstream. It meant I was able to self-test and self-dose whilst my warfarin took effect - a great reassurance and no trips to the vampire.
Of course your mileage may vary depending on valve, cardiologist and hospital - I'm just summarising my experience as best as I can.


