ElectLive
Well-known member
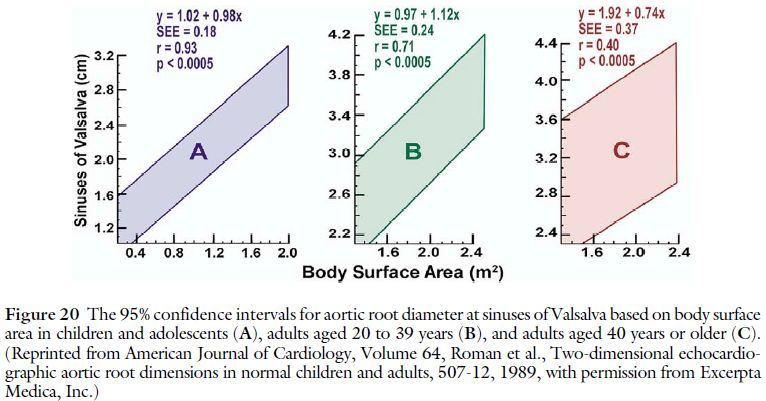
In your experience, is there a difference in echo VS CT without contrast for aortic root? My echo (read) by the same cardio have been very consistent. 4.2, 4.1, 4.2 and 4.2 at the root. The 2nd to last 4.2 was read by someone else as a 3.7 but as stated the 2nd cardio whom did the 1st 2 said he sees a stable 4.2 across all the echo’s. The CT showed a 4.38 at the root without contrast. I was told if I did contrast that may have gotten 4.2 (would have measured just the contrast area) as well as the CT can give larger dimensions due to imaging a moving target as well as the CT # is most accurate…
Chris - Thanks again. You know, my own set of measurements were identical. Interestingly, the measurements themselves are usually not 1 to 1, in other words, echo is internal diameter and CT is external diameter, but as you might guess, it normally doesn't make much of a difference, except sometimes at the descending aorta. I think the only real need for contrast is diagnosing issues of the aorta tissue, such as dissection, it doesn't really impact size measurements much, but the cardiologist's comment makes a lot of sense in that regard, thanks for sharing. For the aorta as a whole, CT and MRI are more accurate, but they come at the expense of being more invasive and expensive, so they are not the initial preferred method. But as I said in the other thread, the root seems to be one place where echo deficiencies are not really true. There is a long discussion in the Aorta Guidelines, referenced above, that describes the pros and cons of each method, in much more detail than my comments.