pellicle
Professional Dingbat, Guru and Merkintologist
Hi
a user here frequently suggests that meters (such as the Coagucheck XS) are designed to be within 30% tolerance. I have always found that an interesting claim and have looked for supporting evidence for that since I first read it.
I have not found anything about the design of meters, but I have found some interesting things about the reference standards which I thought you (the reader) also may find interesting.
The idea of such "accuracy" seems to come from an ISO standard, the Coagucheck XS acceptance test documents say the following:
I feel that what this suggests is that without other guidelines to refer to, Roche has chosen to adhere to the ISO17593 standard which it seems is not so tight. It has been suggested in the literature that this ISO standard is in need of review these days. A 30% range for INR greater than 2 would be between 1.4 and 2.6 With such tolerances it is no wonder that many clinics erred on the higher side (to prevent thrombosis at the risk of bleeds)
It has been said before that many things influence the numbers you get from a lab, everything from how the blood is handled to the 'reagents' used. This article supports that the 'reagents' used in the lab are important variables
I found slide 6 (page 6) of this presentation quite informative here, and it puts into historical context the advances of anticoagulation therapy. Page 10 is also interesting in the presentation of the data suggesting that Labs give higher (increasing with INR) reading than machines. Page 11 suggests that at INR lower than 3 the accruacy is good.
None the less studies comparing these Point Of Care meters has suggested very good results, much more accurate than 30% in the vast majority of cases.
As I posted in this thread the accuracy of home INR machines is significantly better than ±30%
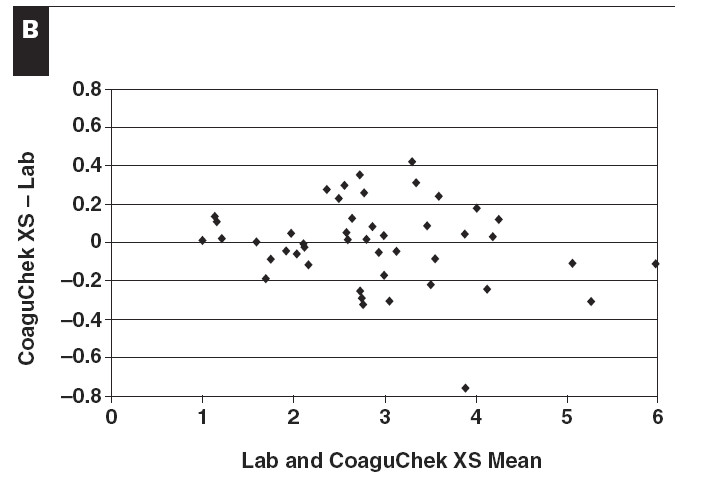
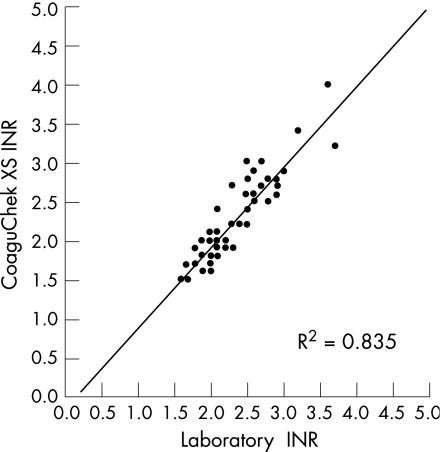
For INR = 3 a 30% variance would be 2.1 to 3.9 yet the above chart shows nothing like that, with only the outliers even approaching that.
My view is that the testing of these meters has shown that they can be relied upon by many, but that there are outliers. So always get reference checks when you start home testing, and perhaps given the variablity of Lab results if you are concerned then get cross referenced results.
If anyone can find a reference to suggest that the current generation of coagulation meters were designed with 30% tolerance in mind I'd appreciate seeing that, however I feel that they are actually designed with much higher accuracy in mind and the compliance to standards is the issue - NB that the standards are too broad.
a user here frequently suggests that meters (such as the Coagucheck XS) are designed to be within 30% tolerance. I have always found that an interesting claim and have looked for supporting evidence for that since I first read it.
I have not found anything about the design of meters, but I have found some interesting things about the reference standards which I thought you (the reader) also may find interesting.
The idea of such "accuracy" seems to come from an ISO standard, the Coagucheck XS acceptance test documents say the following:
Additional evaluation criteria were set for information only according to the
draft ISO standard 17593 [1], which requires a
- mean bias of ≤0.3 INR (in the INR range 2.0 – 4.5) and
- a total of >90% of all data bias within +/- 0.5 INR (for INRs <2) or
within +/- 30% (for INRs >2)
I feel that what this suggests is that without other guidelines to refer to, Roche has chosen to adhere to the ISO17593 standard which it seems is not so tight. It has been suggested in the literature that this ISO standard is in need of review these days. A 30% range for INR greater than 2 would be between 1.4 and 2.6 With such tolerances it is no wonder that many clinics erred on the higher side (to prevent thrombosis at the risk of bleeds)
It has been said before that many things influence the numbers you get from a lab, everything from how the blood is handled to the 'reagents' used. This article supports that the 'reagents' used in the lab are important variables
In conclusion, our data show some important differences are present between INRs determined using Recombiplastin, Innovin and two conventional thromboplastins
I found slide 6 (page 6) of this presentation quite informative here, and it puts into historical context the advances of anticoagulation therapy. Page 10 is also interesting in the presentation of the data suggesting that Labs give higher (increasing with INR) reading than machines. Page 11 suggests that at INR lower than 3 the accruacy is good.
None the less studies comparing these Point Of Care meters has suggested very good results, much more accurate than 30% in the vast majority of cases.
As I posted in this thread the accuracy of home INR machines is significantly better than ±30%
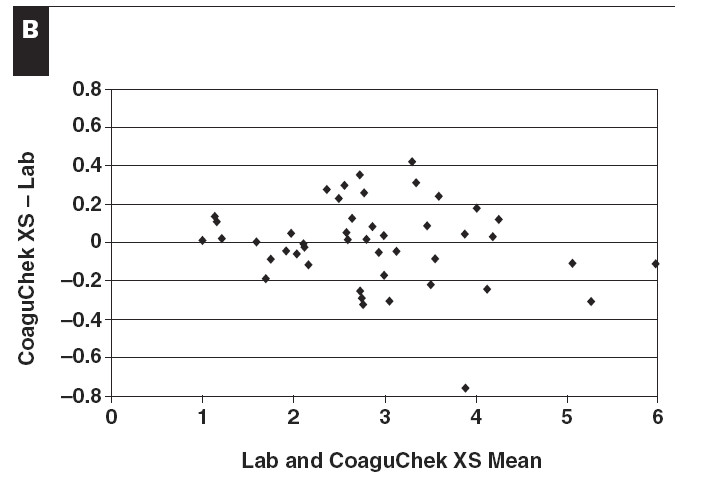
For INR = 3 a 30% variance would be 2.1 to 3.9 yet the above chart shows nothing like that, with only the outliers even approaching that.
My view is that the testing of these meters has shown that they can be relied upon by many, but that there are outliers. So always get reference checks when you start home testing, and perhaps given the variablity of Lab results if you are concerned then get cross referenced results.
If anyone can find a reference to suggest that the current generation of coagulation meters were designed with 30% tolerance in mind I'd appreciate seeing that, however I feel that they are actually designed with much higher accuracy in mind and the compliance to standards is the issue - NB that the standards are too broad.