pellicle
Professional Dingbat, Guru and Merkintologist
Hi
perhaps this is not the correct location to place such a topic, and perhaps there is little anyone can say in responce to this topic. So if a moderator wishes to move it then by all means.
I had my most recent OHS in Nov 2011, I have an Aortic valve replaced with an ATS valve and had a section of my aorta replaced/repaired with a tube of some fabric such as dacron.
All things progressed towards reasonable healing with the exception that I complained of the wires bugging me through out the healing process. Bear in mind I saw no reason to mention this significantly till well past 8 weeks.
Things progressed with some minor aches and pains until November 2012 *(yes a year later) when I found that the upper part of my sternum was beginning to swell.

This progressed to a point where it became obvious to the surgeon that something was amiss. That lead to a surgical 'debridement' of the wound and the removal of the sternal wires on the 23rd of November 2012.

The recovery of the surgical wound has progressed in good time.
Throughout the recovery while the wound looked as perfect as one could hope for in a wound recovery there remained a light greenish discharge coming from the top of the wound, which was actually just short of the manubrium, and the source of the swelling in the first place.
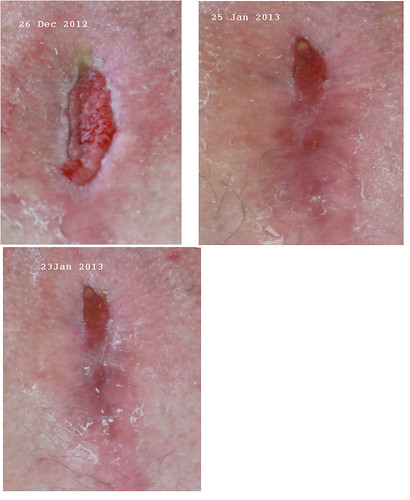
It was clear that a 'discharge' of green liquid which continued to flow (more or less at an unchanged rate) from the top of the wound indicated that an infection lay beneath, even if the wound itself was clear of infection. The wound management people said that the wound itself showed no signs of infection but that the discharge should be viewed as a problem.
The wound has now closed and (surprise surprise) the manubrium is now swelling again.
Right now I am feeling a mixture of emotions which seem to range through anger, despair, frustration, depression and numbness. That I am also still struggling with the totally unexpected and shocking passing of my dearly beloved wife just in August 2012 does not help me to maintain an even keel on all of this.
However I feel that I would like to take this opportunity to remind those who seem to take lightly entering into multiple OHS that you are foolish in the extreme to do so lightly. OHS is a life threatening event, and the recovery is not certain to be straight forward (although most are). Complexity increases (and thus risk) with each successive operation.
Do not take the successful outcomes of one or even two surgeries to beguile you into thinking that its just an arduous process. It is far far more than that. If you have had a straight forward recovery (as indeed my first two were), then give thanks to whatever deity you believe in and do not tempt such deity to intercede for you in the third surgery.
Your doctors/surgeons will (or should) rightly tell you that each sucessive operation multiplies the risks, not the least because of the simple aspect of statistics. The healing of wounds through scar tissue are unlike the initial healing of wounds. Blood flow is different and susceptibility to infection or incomplete healing is more likely.
So to those who consider a tissue valve and re-operation at a later date due to a pathological fear of warfarin anti-coagulation therapy I advise you to consider:
* do you really know what you are talking about with your issues of warfarin?
* if you were in my situation would you wish you'd not had your third?
* is the risk of anticoagulation therapy greater than the risks of post surgical complications?
Naturally there are other reasons why one would be "contra inticated" for a mechanical ...
In my case I had little choice about a third operation. I had my first as a valvotomy when I was a youth, my second as a human tissue implanted valve (homograph) in my late 20's and this third operation (at 48) we considered only a mechanical valve. Both the surgeon and I were not wishing to undertake a fourth.
I have no idea what will come of this next, but I will keep you posted if anyone finds any value in that.
As the kids say "FML"
perhaps this is not the correct location to place such a topic, and perhaps there is little anyone can say in responce to this topic. So if a moderator wishes to move it then by all means.
I had my most recent OHS in Nov 2011, I have an Aortic valve replaced with an ATS valve and had a section of my aorta replaced/repaired with a tube of some fabric such as dacron.
All things progressed towards reasonable healing with the exception that I complained of the wires bugging me through out the healing process. Bear in mind I saw no reason to mention this significantly till well past 8 weeks.
Things progressed with some minor aches and pains until November 2012 *(yes a year later) when I found that the upper part of my sternum was beginning to swell.

This progressed to a point where it became obvious to the surgeon that something was amiss. That lead to a surgical 'debridement' of the wound and the removal of the sternal wires on the 23rd of November 2012.

The recovery of the surgical wound has progressed in good time.
Throughout the recovery while the wound looked as perfect as one could hope for in a wound recovery there remained a light greenish discharge coming from the top of the wound, which was actually just short of the manubrium, and the source of the swelling in the first place.
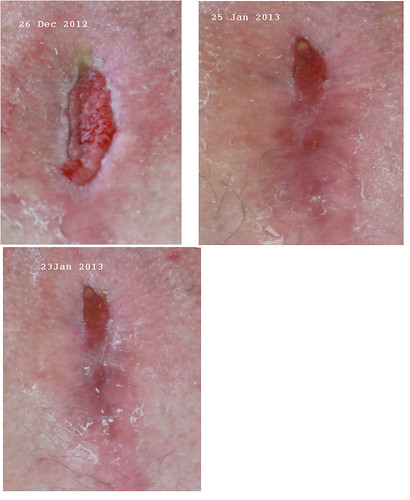
It was clear that a 'discharge' of green liquid which continued to flow (more or less at an unchanged rate) from the top of the wound indicated that an infection lay beneath, even if the wound itself was clear of infection. The wound management people said that the wound itself showed no signs of infection but that the discharge should be viewed as a problem.
The wound has now closed and (surprise surprise) the manubrium is now swelling again.
Right now I am feeling a mixture of emotions which seem to range through anger, despair, frustration, depression and numbness. That I am also still struggling with the totally unexpected and shocking passing of my dearly beloved wife just in August 2012 does not help me to maintain an even keel on all of this.
However I feel that I would like to take this opportunity to remind those who seem to take lightly entering into multiple OHS that you are foolish in the extreme to do so lightly. OHS is a life threatening event, and the recovery is not certain to be straight forward (although most are). Complexity increases (and thus risk) with each successive operation.
Do not take the successful outcomes of one or even two surgeries to beguile you into thinking that its just an arduous process. It is far far more than that. If you have had a straight forward recovery (as indeed my first two were), then give thanks to whatever deity you believe in and do not tempt such deity to intercede for you in the third surgery.
Your doctors/surgeons will (or should) rightly tell you that each sucessive operation multiplies the risks, not the least because of the simple aspect of statistics. The healing of wounds through scar tissue are unlike the initial healing of wounds. Blood flow is different and susceptibility to infection or incomplete healing is more likely.
So to those who consider a tissue valve and re-operation at a later date due to a pathological fear of warfarin anti-coagulation therapy I advise you to consider:
* do you really know what you are talking about with your issues of warfarin?
* if you were in my situation would you wish you'd not had your third?
* is the risk of anticoagulation therapy greater than the risks of post surgical complications?
Naturally there are other reasons why one would be "contra inticated" for a mechanical ...
In my case I had little choice about a third operation. I had my first as a valvotomy when I was a youth, my second as a human tissue implanted valve (homograph) in my late 20's and this third operation (at 48) we considered only a mechanical valve. Both the surgeon and I were not wishing to undertake a fourth.
I have no idea what will come of this next, but I will keep you posted if anyone finds any value in that.
As the kids say "FML"
Last edited:



























