I went to see my new cardiologist two weeks ago and he hits me hard with - your going to need your aortic valve replaced, not right now, but we need to start a 6 month echo schedule. I was floored and have been through a whole range of emotions since then.
The murmur was first heard in my early 20s, I'm 54 now. I had a few echos done 20 years ago and they were stable, not much change. So, I went on with my life and didn't even think about it. I'm in the best shape of my life, good blood lipid profile, but on Lisonopril for HBP. I have no symptoms, which is good.
Fast forward to 2007 and the first bout of A-Fib. New echo and a transesophageal echo at that time. The aortic valve is trileaflet, but calcified. I get set up with a great electrophysiologist at CVM - Davenport (IA) at that time. I love this guy. I've had two other A-fibs since then and his message to me is - "get out of here and make room for the sick people". He decides to leave to teach and the practice wants me to start with a 'plumber', not just an 'electrician'.
So, I go to the 'plumber' and let's just say bedside manner isn't his strong suit. He was quite brusque in his message and it was very upsetting for myself and my spouse. I will admit that the echo results did get worse in the last year. Here they are:
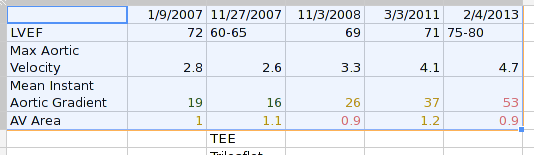
I guess I've progressed from "moderate stenosis" to "severe". How long until I'm critical?
So, I'm tied up in knots over when I'll have to do OHS. I have an appt set up with the Univ of Kansas Med Center in Kansas City in three weeks for more information and another echo. My wife is from that area and we have more support network there. I'm not thrilled about driving that far, especially if I decide to have surgery there, but it's for the best.
I've already decided that when I go back to CVM that I'll be asking for a different Dr. This is just too important.
I have a TON of questions and will start posting these as I can. Actually, this document helped a lot, especially the 'decision tree' on p. 721. Thanks for your time and support.
The murmur was first heard in my early 20s, I'm 54 now. I had a few echos done 20 years ago and they were stable, not much change. So, I went on with my life and didn't even think about it. I'm in the best shape of my life, good blood lipid profile, but on Lisonopril for HBP. I have no symptoms, which is good.
Fast forward to 2007 and the first bout of A-Fib. New echo and a transesophageal echo at that time. The aortic valve is trileaflet, but calcified. I get set up with a great electrophysiologist at CVM - Davenport (IA) at that time. I love this guy. I've had two other A-fibs since then and his message to me is - "get out of here and make room for the sick people". He decides to leave to teach and the practice wants me to start with a 'plumber', not just an 'electrician'.
So, I go to the 'plumber' and let's just say bedside manner isn't his strong suit. He was quite brusque in his message and it was very upsetting for myself and my spouse. I will admit that the echo results did get worse in the last year. Here they are:
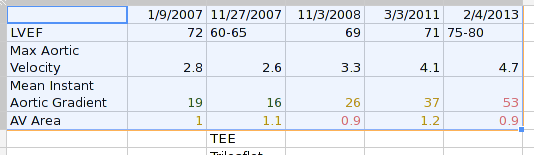
I guess I've progressed from "moderate stenosis" to "severe". How long until I'm critical?
So, I'm tied up in knots over when I'll have to do OHS. I have an appt set up with the Univ of Kansas Med Center in Kansas City in three weeks for more information and another echo. My wife is from that area and we have more support network there. I'm not thrilled about driving that far, especially if I decide to have surgery there, but it's for the best.
I've already decided that when I go back to CVM that I'll be asking for a different Dr. This is just too important.
I have a TON of questions and will start posting these as I can. Actually, this document helped a lot, especially the 'decision tree' on p. 721. Thanks for your time and support.
























