Hi
WillyWarfarinWizard
I'm on my 2nd valve replacement my first was a human one, this one is a mechanical. I manage my own INR too. I see many of your questions are actually really "classics" in warfarin management. I hope that my reply helps
WillyWarfarinWizard;n862296 said:
I'm currently managing my INR in the 2.5 - 3.5 range as required. I manage this with 7.5 - 8.0 mg Warfarin each day.
that's a slightly higher range than is usual for an Aortic valve, do you have some other conditions which make stroke more likely? If not I'd question why you're higher than both the USA and European Surgical Guidelines for post operative management (which is 2 ~ 3).
I get my INR measured at the lab on Mondays and home test with a Coaguchek XS meter on Friday.
this is also a bit unusual as you are essentially being measured twice per week. I can see little benefit for that, although I'm a strong supporter of weekly measurements and bi-weekly if you are monitoring something. If you're having them checked twice weekly for the purposes of seeing if readings are the same between your home test and the INR at the lab, then you will be better off doing them within hours not days.
My physician mentioned to me my INR seems to be more prone to change than most of his patients.
without knowing your doctor I'll say that most doctors have so little actual knowledge on INR management that its embarrassing. I would take that with a grain of salt.
Firstly how long since your surgery? For the first year on warfarin you can see all manner of variations as your body reacts to the surgery and healing post surgery. I wonder how many of his other patients that are on warfarin are elderly and taking warfarin for stroke history or thrombosis? I'd say the majority.
He also mentioned my dose is slightly higher than most patients who typically take 5 -6 mg/day.
Unimportant, its like saying most of his patients are older and you're younger ... so what? The thing is we all have different metabolisms, and the whole point of warfarin is to adjust coagulation levels for YOU. So if you're a size 9mg man then just wear a size 9 and be happy. The amount of warfarin we take has only one real outcome - proper coagulation. Any perceptions of taking less for any other reasons are unfounded.
I'm very active and can say I'm the same weight when I was 16 and I like to eat different foods.
I can't claim the same weight, but I'm quite active for a 50YO .. I see in your Bio about your outdoor work and when I'm back in Finland (I'm in Australia now) I XC Ski almost every day that I can (which is usually from late Dec through till April) and cycle through out the year. In Finland I don't own a car and walk / cycle around town.
Eating food has far less impact than the internet will have you believe. If you search here you'll find many of us see little variation in INR that can be correlated with food. Although lay off the Grapefruit juice!
I limit my alcohol consumption to 2 drinks/day with one day/week off. I once had a "culinary misadventure" where I consumed approximately 5 - 6 glasses of wine followed up with a glass of cask strength single malt. My INR shot up to 4.7 from 2.7
Its hard to be sure that the drinking was the cause. I mean in science its well established to have a control (where no alcohol is taken) and at the same time an experimental (where alcohol is taken). Given that your INR can fluctuate its hard to be sure that THAT was the cause.
also, of and in itself 4.7 is just outside the safe zone, so don't panic there.
I skipped a days dose and managed to lower my INR to 3.6 the next day and to 2.5 the following day.
the important thing to remember with INR and warfarin is that its like a bucket with a hole in it: if you pour water in faster than the hole drains it, then water accumulates in the bucket. Slower and the bucket empties.
The hole for warfarin is your P450 pathway (liver related disposal) and so it can't pull out warfarin instantly. So the disposal rate is measured in half life. So half of what you took is disposed of in 48 hours. Because you'll also be taking more within 24 hours your getting more to top that bucket up.
So the key is "how big is your warfarin disposal rate" because it isn't exactly 48 hours and varies from person to person.
This is why we measure INR, because we can see from our INR (the only thing we are interested in really) that once the levels settle we know what we need to be adding to the bucket to keep an even level.
I say this because your monitoring and redosing strategy is going to result in over corrections (like a kid doing a tail slide on an ice track) ... you want to balance that slide. Over correcting won't help. There is an "old adage" that warfarin takes a week to react. The detail of the adage is wrong, but the message is correct. Leave it a week to be sure what its settling to.
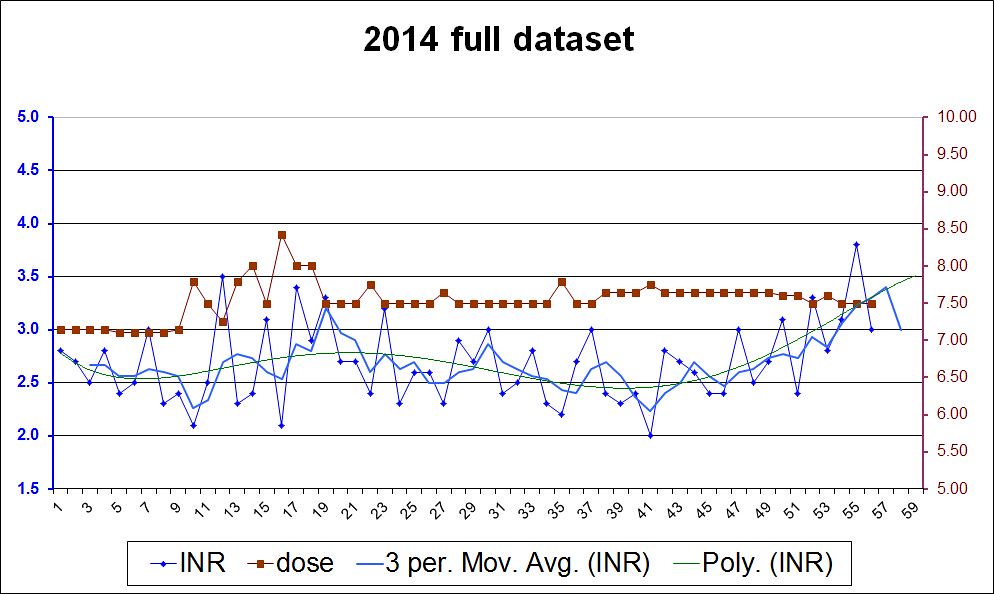
I use a spread sheet and a graph to assist me. If you'd like to discuss that please use the message system here and get in touch.
My target is 3.0 - 3.5 and manage that by taking 7.5 mg/day for 2 days and 8.0 mg. on the 3rd day. If my INR trends up, I will go 3 days at 7.5 mg before I take 8.0 mg. If my INR trends down, I will alternate between 7.5 & 8.0 mg until I reach my range.
,
I think you're on a good method there, I feel that its important to keep the dose variations small such as you are. Myself I now make weekly changes of about 0.5 or 0.25mg if needed ...
I've got a few other points of interest to discuss if you're interested. I also use skype, so if you want we can chat about things (often easier than typing)
Best Wishes