Finally got out of the hospital yesterday, on post-op day 6, after my INR reached 2.2 from 1.5, with the help of a heparin drip for almost 24 hours. There was some confusion with the surgeon’s nurse who for some reason thought my range should be 2.0-3.0, with a mechanical valve (not on-x) - if not for that I might still be there now, instead of relaxing at home with a cup of tea, in my own clothes, in the quiet; no more being stuck and poked and tortured by the phlebotomy sadists & nurses on power trips that walk the halls. I need to remember that good things can also come from other people not knowing what they’re talking about, ha ha.
A question: they wanted me to reduce my warfarin dose last night from 5 to 2.5, before returning to 5 tonight... Even if my range really was 2.0-3.0, having had a last INR of 2.2, would thatve been the right thing to do?... Were they expecting / Are there late effects from the heparin?
I took 5 mg. With a twinge of conscience from disobeying my very first order for my first experience dosing Warfarin...
Any thoughts?
Thank you, guys.
Heparin should not be detected in an INR number, there is separate blood reading they do for how effective Heparin is. If you range is 2-3 and you are at 2.2 Why do they want to you half your dose. One frustration I have with the INR people was the constant dosage tweaking and the alternating doses they wanted me taking. I like predictable dosing. I eventually stopped using the service becasue my PCP will write my scripts now. She knows how anal I am about this stuff and I have a spreadsheet over the last 2 years since my surgery showing every dose and every reading I took.
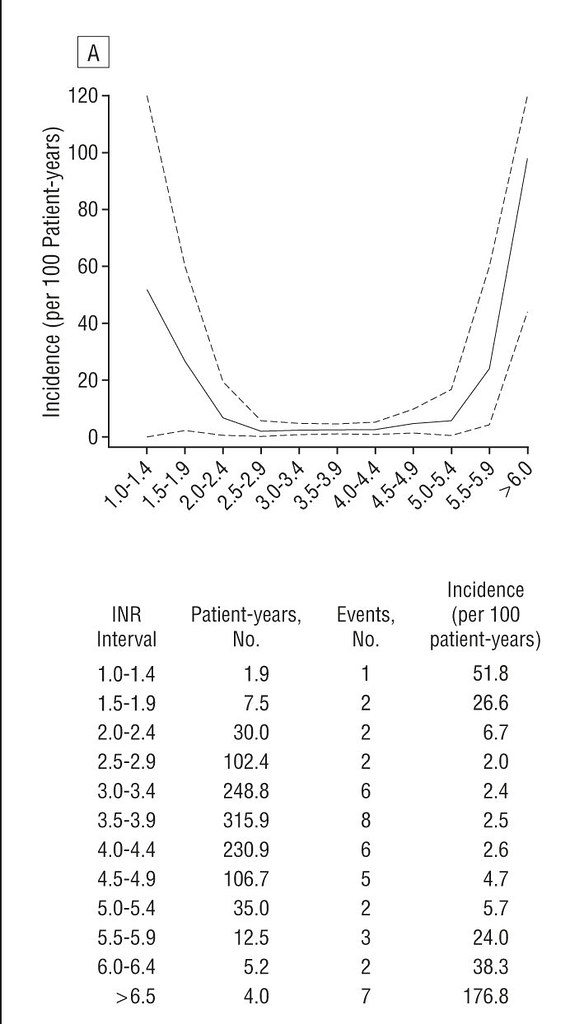
I was taking 6.75 daily (a 4mg and a 1/2 of a 7.5mg )for a long time and while I had swings they were always in range. I have an On-X and take a daily 81mg aspirin and I use 2.0-3.0 as my range and my cardio agreed to that. I very rarely fall below 2. 5, btu occasionally get as high as 3.4. If you look ta the atts (posted somewhere on this forum) the sweet spot is 2.5-3.0 but going a little over does not change the risk much. Late last years I was running low liek 2.1-2.2 so I moved my does up to 7.5, but lately I have had more 3.1-3.4 reading that I care for so I have gone to 1-2 days week I take 1/2 of a 7/5mg until I see if I need to go back to 6.75 or get something in line with 7.0-7.25. I don't want to be mixing and splitting a bunch of pills so right now the 1-2x a week split my 7.5 will work until I see the new trend.
Most people can expect a dose change to impact in about 3 days, my body is more like 1 week or more.