- Joined
- Dec 5, 2020
- Messages
- 2,791
This was published last month: August 2021.
I have found no evidence that the guidelines for mechanical St Jude in the aortic postion have changed. I have been given the range of 2.0-3.0. The below publication is current and recommends a target of 2.5 for St Jude. This would be consistent with the range I was given of 2.0-3.0.
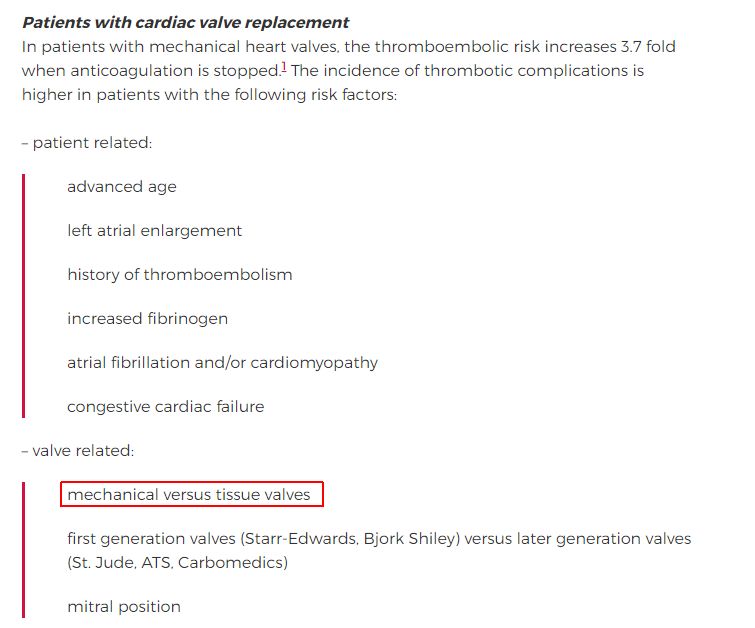
" For patients with an On-X mechanical bileaflet aortic valve with no other risk factors for thromboembolism, we suggest anticoagulation with a VKA to achieve an INR range of 2 to 3 for the first three months after valve surgery; after three months, the goal INR range is 1.5 to 2. "
" For patients with a bileaflet (other than On-X) or single tilting disk mechanical aortic prosthetic valve with no other risk factors for thromboembolism, we recommend anticoagulation with a VKA to achieve a target INR of 2.5. "
" For patients with a mechanical aortic prosthetic valve (other than On-X) and an additional risk factor for thromboembolic events (AF, previous thromboembolism, left ventricular (LV) systolic dysfunction, or hypercoagulable condition) or an older generation mechanical aortic valve prosthesis (eg, ball-in-cage), we suggest anticoagulation with a VKA to achieve an INR of 3. "
https://www.uptodate.com/contents/a...valves in both the aortic,a target INR of 2.5.
I have found no evidence that the guidelines for mechanical St Jude in the aortic postion have changed. I have been given the range of 2.0-3.0. The below publication is current and recommends a target of 2.5 for St Jude. This would be consistent with the range I was given of 2.0-3.0.
" For patients with an On-X mechanical bileaflet aortic valve with no other risk factors for thromboembolism, we suggest anticoagulation with a VKA to achieve an INR range of 2 to 3 for the first three months after valve surgery; after three months, the goal INR range is 1.5 to 2. "
" For patients with a bileaflet (other than On-X) or single tilting disk mechanical aortic prosthetic valve with no other risk factors for thromboembolism, we recommend anticoagulation with a VKA to achieve a target INR of 2.5. "
" For patients with a mechanical aortic prosthetic valve (other than On-X) and an additional risk factor for thromboembolic events (AF, previous thromboembolism, left ventricular (LV) systolic dysfunction, or hypercoagulable condition) or an older generation mechanical aortic valve prosthesis (eg, ball-in-cage), we suggest anticoagulation with a VKA to achieve an INR of 3. "
https://www.uptodate.com/contents/a...valves in both the aortic,a target INR of 2.5.
Last edited: