I'm seeking advice and suggestions regarding warfarin protocols and alternative options to bridging with lovenox prior to and following arthroscopic surgery to repair a torn meniscus. I've read other posts on this subject in general (thank you especially pellicle) but I am interested in knowing if there are other viable options for this type of surgery, which I understand is relatively simply and quick, like 20 minutes. I've yet to coordinate with my cardiologist and PCP because I value the experience and insights from you folks even more, although I'm not sure I'm going to have much of a choice in the matter. I have a mechanical valve in the mitral position, self-test, and maintain an INR close to 3.5. My torn meniscus is sitting in a swollen pool of mostly blood, by the way.
You are using an out of date browser. It may not display this or other websites correctly.
You should upgrade or use an alternative browser.
You should upgrade or use an alternative browser.
Anti-coagulating with torn meniscus
- Thread starter QuincyRunner
- Start date

Help Support Valve Replacement Forums:
This site may earn a commission from merchant affiliate
links, including eBay, Amazon, and others.
pellicle
Professional Dingbat, Guru and Merkintologist
I'd follow my protocol here
https://cjeastwd.blogspot.com/2017/12/perioperative-management-of-inr.html
I sort of did for my foot surgery, but the surgeon said he doesn't care because he excludes blood with a pressure system
https://cjeastwd.blogspot.com/2020/10/another-example-small-procedure.html
I believe it's well manageable.
Reach out if you want to chew the fat.
Best Wishes
PS
thanks
https://cjeastwd.blogspot.com/2017/12/perioperative-management-of-inr.html
I sort of did for my foot surgery, but the surgeon said he doesn't care because he excludes blood with a pressure system
https://cjeastwd.blogspot.com/2020/10/another-example-small-procedure.html
I believe it's well manageable.
Reach out if you want to chew the fat.
Best Wishes
PS
(thank you especially pellicle)
thanks
pellicle
Professional Dingbat, Guru and Merkintologist
oh, and based on my reading of the GELIA study (and these guys too)
https://academic.oup.com/eurheartjsupp/article/3/suppl_Q/Q39/612272
there would seem to be not any significant risk associated with short duration lower INR (like 1.4)
as indicated in this study (also agnostic of valve position)

URL for study
http://jamanetwork.com/journals/jamainternalmedicine/fullarticle/415179
lets say that you take the 50 incidents per 100 patient years, that would mean that if you were INR 1 <> 1.4 that you could statistically anticipate an incident if you stayed that way for a year. In less than a week I'd be surprised. Thus the guys I cited in my colonoscopy prep said:
I would print out those journal articles and take them to your team.
I hope the surgery goes well
https://academic.oup.com/eurheartjsupp/article/3/suppl_Q/Q39/612272
there would seem to be not any significant risk associated with short duration lower INR (like 1.4)
as indicated in this study (also agnostic of valve position)

URL for study
http://jamanetwork.com/journals/jamainternalmedicine/fullarticle/415179
lets say that you take the 50 incidents per 100 patient years, that would mean that if you were INR 1 <> 1.4 that you could statistically anticipate an incident if you stayed that way for a year. In less than a week I'd be surprised. Thus the guys I cited in my colonoscopy prep said:
Do the benefits of anticoagulation outweigh the risks?
The approach to the management of anticoagulation in patients with prosthetic valves undergoing non-cardiac surgery remains controversial. The need for perioperative anticoagulation in patients with mechanical heart valves has been questioned in a recent review. The authors argue that for every 10 000 patients with mechanical heart valves who are given perioperative intravenous heparin, three thromboembolic events are prevented at the cost of 300 major postoperative bleeding episodes
I would print out those journal articles and take them to your team.
I hope the surgery goes well
I underwent this surgery and my surgeon discussed the risks of a bleed which he considered not significant. The surgery was completed without a change in my warfarin therapy. Best of luck to you on your journey.
I'm seeking advice and suggestions regarding warfarin protocols and alternative options to bridging with lovenox prior to and following arthroscopic surgery to repair a torn meniscus. I've read other posts on this subject in general (thank you especially pellicle) but I am interested in knowing if there are other viable options for this type of surgery, which I understand is relatively simply and quick, like 20 minutes. I've yet to coordinate with my cardiologist and PCP because I value the experience and insights from you folks even more, although I'm not sure I'm going to have much of a choice in the matter. I have a mechanical valve in the mitral position, self-test, and maintain an INR close to 3.5. My torn meniscus is sitting in a swollen pool of mostly blood, by the way.
I have f-ed up knees too. Make sure you really need the surgery. Make sure you know the success rate of the surgery compared to other treatments. Get a second or even third opinion. For my last knee incident I saw two orthopedists and my PCP. Many orthopedic surgeons do not use alternative routes such as NSAIDs, physical therapy and use of a brace (Donjo brand is my favorite). I chose that route for now, knowing I will need replacement knees in the future. When I get re-injured, they remove fluid every so often with a big needle in the doctor's office. Usually not more than 2-3 times. Your pool of blood is probably impacted by your INR. At an INR of 2-2.5, my last time the first fluid removal had blood but not the second.
I've had surgery on warfarin and the bridging etc. is done per cardiologists orders. They base their decision on valve type and position plus the risk of clots not only from the valve but from the surgery itself.
Thank you Pellicle for all of the reference material and your experiences related to warfarin adjustments and juggling the opposing risks of bleeding and thromboembolic events. If I had the aortic valve I would be willing to discontinue the warfarin and let my INR drop without any bridging. With the mitral valve I am still somewhat conflicted. On the other hand Starrman's post indicates that he never even stopped his warfarin and successfully went through knee surgery without any apparent bleeding issues.
Starrman - what was your INR at the time of surgery?
And Tom in Mo - thanks for your response too. I think your knee issues are more serious than mine, although I do know for a fact that I need surgery. The MRI tells me so, not to mention the severe pain the past 3 weeks whenever I bend my knee. I'm walking like Frankenstein and wearing a DonJoy brace when not packing my knee in ice.
Starrman - what was your INR at the time of surgery?
And Tom in Mo - thanks for your response too. I think your knee issues are more serious than mine, although I do know for a fact that I need surgery. The MRI tells me so, not to mention the severe pain the past 3 weeks whenever I bend my knee. I'm walking like Frankenstein and wearing a DonJoy brace when not packing my knee in ice.

$27.99 ($0.23 / Count)
$34.99 ($0.29 / Count)
HerbaMe Heart Support and Blood Pressure Supplement, 120 Capsules, Promotes Cardiovascular Health, Healthy Cholesterol, Triglyceride, Homocysteine, CRP Levels | Natural Artery Cleanse and Protect
Global Pro Sales

$33.75 ($0.38 / Count)
Snap Supplements Heart Health Supplements and Blood Circulation Supplements, 90 Capsules
Sthenos Solutions

$49.00
$62.95
Echocardiography: A Practical Guide for Reporting and Interpretation, Third Edition
Apex_media🍏

$28.91 ($0.32 / Count)
NutraPro Healthy Heart - Heart Health Supplements. Artery Cleanse & Protect. Supports Healthy Cholesterol and Triglyceride. GMP Certified
Gulliver Group
pellicle
Professional Dingbat, Guru and Merkintologist
Hey mate, no worries

Best wishes for a good outcome.
I understand, and its very much a personal decision. You may note I took a heparin shot while waiting for my INR to come up ... might be worth a shot...If I had the aortic valve I would be willing to discontinue the warfarin and let my INR drop without any bridging. With the mitral valve I am still somewhat conflicted...

Best wishes for a good outcome.
pellicle
Professional Dingbat, Guru and Merkintologist
Oh @QuincyRunner , have you ever measured what happens if you miss 1 or 2 doses?
Might be worth an experiment, I'd measure every second day after missing the second dose. Dunno if you test weekly but if you do you could schedule the experiment to commence the day after your regular test it will cost no more than two strips.
Might be worth an experiment, I'd measure every second day after missing the second dose. Dunno if you test weekly but if you do you could schedule the experiment to commence the day after your regular test it will cost no more than two strips.
Christyleedh
Active member
- Joined
- Oct 22, 2021
- Messages
- 26
I posted this in another thread about choosing mechanical or tissue valve, but it’s probably more relevant here:
I had a uterine ablation- which my local doctor probably should never have performed while I was on blood thinners, but a few days after, I started hemorrhaging and needed 7 blood transfusions, and it wasn’t until I was transferred to cleveland clinic by ambulance that they were able to make it stop. This isn’t to scare anyone, but make sure if you choose mechanical, and you take warfarin- get a second opinion before doing an elective procedure if a doctor thinks you can have it without stopping warfarin. I’m sure the nature of the procedure matters.
I had a uterine ablation- which my local doctor probably should never have performed while I was on blood thinners, but a few days after, I started hemorrhaging and needed 7 blood transfusions, and it wasn’t until I was transferred to cleveland clinic by ambulance that they were able to make it stop. This isn’t to scare anyone, but make sure if you choose mechanical, and you take warfarin- get a second opinion before doing an elective procedure if a doctor thinks you can have it without stopping warfarin. I’m sure the nature of the procedure matters.
pellicle
Professional Dingbat, Guru and Merkintologist
really good advice.before doing an elective procedure if a doctor thinks you can have it without stopping warfarin. I’m sure the nature of the procedure matters.
I hope that you're ok now.
Christyleedh
Active member
- Joined
- Oct 22, 2021
- Messages
- 26
Thanks- I am from that complication!really good advice.
I hope that you're ok now.
pellicle
Professional Dingbat, Guru and Merkintologist
life as we age seems to be a series of "complications" which are there to solve.I am from that complication!
Best Wishes
- Joined
- Dec 5, 2020
- Messages
- 2,791
I had a uterine ablation- which my local doctor probably should never have performed while I was on blood thinners, but a few days after, I started hemorrhaging and needed 7 blood transfusions
Hi Christy,
Really sorry to hear that your anti-coagulation was not addressed before your surgery. It certainly should have been considered. I believe that for uterine ablation that RFA is used (radio frequency ablation). Is that correct?
I have had a radio frequency ablation procedue to ablate a benign thyroid goiter and will likely have another one later this year. For my first procedure three years ago I was not on warfarin, but I am now. For my potential upcoming procedure, in my recent consultation, I was told that with RFA bleeding occurs and that the standard of care is to bridge the warfarin with heparin.
The link below seems to agree that it needs to be addressed before uterine ablation:
"In the 2 weeks before your procedure:
- You may need to stop taking drugs that make it hard for your blood to clot. These include aspirin, ibuprofen (Advil, Motrin), naproxen (Naprosyn, Aleve), clopidogrel (Plavix), and warfarin (Coumadin). Your provider will tell you what you should or should not take."
https://ufhealth.org/endometrial-ablation
I guess the take away is that all of us need to be our own advocate and be aware that we should ask a lot of questions if we have a procedure of any type coming up and are on warfarin. Unfortunately, it seems that some clinics are not up to speed on the standards of care.
Glad that you got the care you needed to take of the bleeding at the Cleveland Clinic.
Pellicle - I have never purposefully skipped a dose, let alone two. However, I do test weekly and I think I will try skipping a dose after my next test and then test again a day or two later. I'm not sure that I have the nerve to skip two days in a row, although it would be nice to see how fast my INR drops and to what level.
Christy -Thank you for sharing your story, and for the scary example of the danger inherent in being overly anti coagulated going into surgery. It is shocking to me that your cardiologist or your primary care doctor, both of whom should have known better, did not intervene on your behalf with the ignoramus that did your procedure.
Christy -Thank you for sharing your story, and for the scary example of the danger inherent in being overly anti coagulated going into surgery. It is shocking to me that your cardiologist or your primary care doctor, both of whom should have known better, did not intervene on your behalf with the ignoramus that did your procedure.
pellicle
Professional Dingbat, Guru and Merkintologist
I sort of started out with accidents of memory and took advantage of my machine to measure (especially when it was within a day or so of my regular measurement day).have never purposefully skipped a dose, let alone two. However, I do test weekly and I think I will try skipping a dose after my next test and then test again a day or two later. I'm not sure that I have the nerve to skip two days in a row, although it would be nice to see how fast my INR drops and to what level.
This accumulated knowledge made me curious to try two days (which could in theory happen), as I knew **** had experience in that regard and it took him over 5 missed days with a ball and cage type valve which has a much higher thrombosis generation capacity.
Test and know thyself
Quincy - I don't know what it was that day….but the range is 2.0-3.0. I followed my surgeon’s advice. Mine was arthroscopic procedure clearing out a lot of damaged cartilage and scar tissue. If it was was a full knee replacement or a more complex procedure, I would imagine the surgeon advice would have been different.
Starrman - thank you for that information. It gives me hope that I can go through my surgery without any major adjustments to my warfarin regimen.
Pellicle - well, in order to "know myself" as you suggested, I skipped my dose last night (Sunday) after testing with a 3.2 INR. I will skip again tonight and I see no need to test again tonight since my missed doses won't show up in my INR this quickly. I think I will test tomorrow night and if my INR is still over 2 I may even skip a 3rd night. What do you think? And when I start back from a low INR, say 1.5, should I just go back to my nightly dose of 7.5 and assume that I will be back in range by Sunday?
Pellicle - well, in order to "know myself" as you suggested, I skipped my dose last night (Sunday) after testing with a 3.2 INR. I will skip again tonight and I see no need to test again tonight since my missed doses won't show up in my INR this quickly. I think I will test tomorrow night and if my INR is still over 2 I may even skip a 3rd night. What do you think? And when I start back from a low INR, say 1.5, should I just go back to my nightly dose of 7.5 and assume that I will be back in range by Sunday?
pellicle
Professional Dingbat, Guru and Merkintologist
well I think you should just skip one, then test at the interval I mentioned (which would be a measurement and of course a previous weeks measurement also know. Lets call that Monday. Then miss a dose Tues, measure Wed, measure Fri). From there that willI may even skip a 3rd night. What do you think?
- inform you as to what happens and how long it takes to recover
- will not be an onerous or risky experiment
- to me "rules of thumb" on how long things take are one thing, actual measurements are even better
- if you are inclied to share the data with me I can plug it into my model and see if what you observe conforms to my model or not. If it does then happy days.
Last edited:
Pellicle - Well I didn't exactly follow your suggested plan but I did learn that my INR drops faster than I expected, and faster than yours did as charted in your preoperative management of INR blog in which your INR dropped from around 2.3 to around 1.2 after 4 days of missed doses. I started from a higher INR of 3.2 on Sunday but dropped to 1.6 tonight after only two missed doses on Sunday night and Monday night. I took 10 mg of warfarin tonight (higher than my 7.5 normal dose) and will probably take the increased amount again tomorrow night. I realize that I will drop below 1.6 tomorrow night because of the lag affect but I don't feel too panicked. I drank some grapefruit juice tonight to speed things up and I am going to take some ibuprofen tonight to both increase my INR and as a bonus to help with the pain and inflammation associated with my torn meniscus. If I end up getting a blood clot before my INR gets back in therapeutic range I will post the unfortunate result - or not. 
pellicle
Professional Dingbat, Guru and Merkintologist
err ... that's why I suggested what I suggested. And ,as you have a higher dose than me, I would anticipate a faster drop. Hit me up by pm if you wish to know why I anticipate that.2.3 to around 1.2 after 4 days of missed doses.
Anyway I recommend you take one double dose pretty soon and then resume on normal. It will be interesting to see the results of how long it takes to come back up, but either way you now have a good result from with which to estimate your drop.
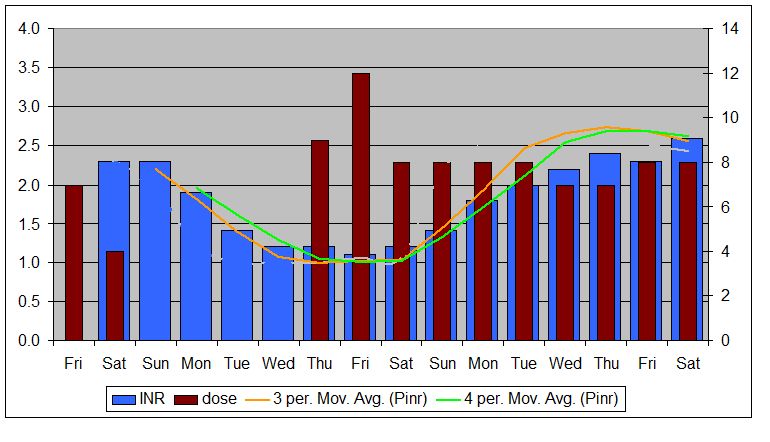
reviewing that lest say that my day of cessation was Sun and INR was about 2.4, it dropped to 1.4 in 3 days and once you look at 4 days it was 1.4. I'm pretty sure you'll find it drops faster from the higher INR and slows down once you get closer to 2 and of course its like a slow landing down to 1 from there.
Also you will probably still keep dropping after you resume, although once it hits 1.0 it of course can't drop more. For you, your un-anticoagulated state may not be 1.0 it may be anything from 1.2 to 0.8 ... it all depends (on where you sit relative to the N in INR).
Thanks for sharing


















